Staff Report
Remember Tootsie Pops from your childhood days? The mega-blob of chewy chocolate in the center resonates with generations as the quintessential example of a sweet spot. Of course, golfers and baseball players dream of finding the fabled sweet spots in their putters and bats. Sweet spots in ophthalmic dispensing are useful tools that can help patients understand adaptation as well as how to get the best from their new lenses.
An ophthalmic lens gives its best performance when the line-of-sight passes through its optical center (OC). For lenses without prescribed prism, the OC is synonymous with the Major Reference Point (MRP). When the lines-of-sight pass through any point away from the OCs or MRPs, there is a reduction in eyewear performance which may or may not be perceptible to the patient.
Every ECP would like to fit lenses that perform equally well throughout their surface area. However, this is beyond today’s technology for many lens prescriptions, particularly for mid-range or higher powers depending on the sensitivity of the patient and the viewing demands. Because of this, the positioning of the MRPs when filling lens prescription is very important. Most ECPs are meticulous in measuring PDs and providing monocular PDs. When ordering, however, the PD only specifies the lateral location of the MRP. The vertical positioning is so often neglected when prescription lenses are ordered that labs simply place the MRP on the datum (mounting) line or a few millimeters above the seg line for lined lenses.
DEFINING THE SWEET SPOT
Most ECPs who use the term sweet spots understand that if the patient perceives the lens performance is reduced whether by blurring, diplopia, or a sensation of discomfort or strain, when viewing through peripheral areas of the lenses the major ray bundles are outside the sweet spots of those lenses. If the performance is perceived to be the same as is experienced when the lines-of-sight are passing through the MRPs, then it can be said that they are within the sweet spots.
A working definition of the sweet spot in an ophthalmic lens is: That area of an ophthalmic lens that gives a performance as perceived by the wearer as equivalent to the performance achieved when the line of sight is passing through the MRP. The size of these areas change with lighting, viewing distance, pupil size and possibly with some psychological and perceptual factors.
For practical purposes the location of the sweet spot for distance seeing is usually centered on the MRPs or OCs for single vision lenses and on or near the DRPs (Distance Reference Points) for PALs. Lenses can be ordered so that the optical centers of a PAL are above the Fitting Crosses. This tends to increase lens thickness and weight, and may thicken the bottom edge of minus lenses and increase the center thickness, weight and magnification of plus lenses.
PERIPHERAL ABERRATIONS
If the refraction is correct, both binocular and monocular vision through the MRPs is usually not a problem. Difficulties in these cases are likely to relate to viewing through the peripheral lens areas. Of the five Seidel Aberrations—Spherical Aberration, Coma, Marginal Astigmatism, Power Error and Distortion—only two can be effectively addressed in ophthalmic lenses by changing the lens curvatures. Lens designers can either address Marginal Astigmatism or Power Error, or they can use curvatures that partially correct both.
Chromatic Aberration also affects the performance of ophthalmic lenses. This is generally worse at longer viewing distances, when excessive decentration is needed, when larger lenses are fitted, or when the patient does critical viewing at long distances.
As shown in Fig. 1, parallel rays of light shown by the broken white lines enter the lens and remain undeviated until the posterior lens surface is reached. At that surface, they are bent, deviating away from the lens’ optic axis which is shown by the solid white ray. The white ray passes through without deviation. The chromatic aberration of the lens causes the peripheral emerging rays to spread with the red rays being deviated least, and the blue rays being deviated most. Entering rays are separated by 1 cm so entering the lens closest to the optic axis emerge with the green ray bent by 6∆, and red and blue rays are separated by the power of the lens divided by its Abbe value (in this case 30) or .2∆. Red rays 1 cm from the optic axis will be bent by only about 5.9∆, while the blue rays will be bent by about 6.1∆. The separation of the colors become greater as the light travels from the lens, and also as entering rays further from the OC are considered. It is this effect that makes images of distant objects more blurred by chromatic aberration than images of objects nearby. The deviations of the green rays are according to Prentice’s Rule using the Helium d-line (587.56 nm) to measure the lens power.
Chromatic aberration is not usually much of a problem for reading and office work. Using lens materials with higher Abbe values, as well as fitting frames at shorter vertex distances can also help.
FIGURE 1
Parallel rays of light shown by the broken white lines enter the lens and remain undeviated until the posterior lens surface is reached. At that surface, they are bent, deviating away from the lens’ optic axis which is shown by the solid white ray. The solid white ray passes through without deviation. The chromatic aberration of the lens causes the peripheral emerging rays to spread with the red rays being deviated least, and the blue rays being deviated most.
BINOCULARITY
The eyewear for every binocular patient should permit at least one viewing angle which permits both lines-of-sight to simultaneously intersect with the sweet spots of their respective lenses. In most cases, that means that the distance binocular PD must be accurate. Occasionally problems arise when the sum of the monocular PDs fails to equal the full distance PD or more often when the vertical heights of the MRPs are left unspecified.
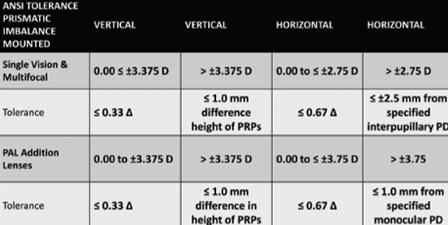
When PDs are taken with a pupilometer, the distance PD may be accurate, but if the bridge of the fitted frame does not center on the pupillometer’s resting point when measurements are made, the monocular PDs will be inaccurate (Fig. 2). This may not cause problems for lower power prescriptions, since a slight head turn to the left or right will generally permit the wearer to simultaneously view through his MRPs.
FIGURE 2
PRESBYOPIA
The concept of sweet spots is more important for bifocals, trifocals and PALs. These lenses should allow clear binocular vision for distance, near and intermediate distances. For patients with prescribed prism, the MRP would be the logical and sweet spot location. But for prism lenses, some patients may discover that an “off MRP” point used monocularly might give an improvement in distance vision.
FIGURE 3
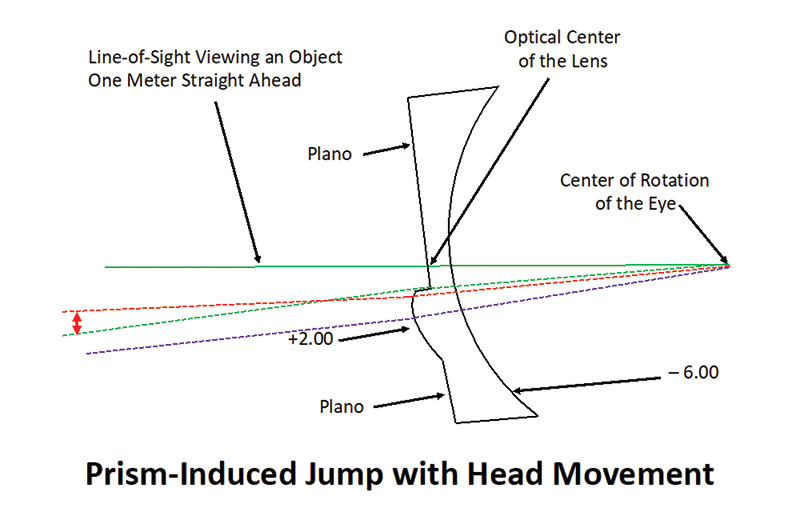
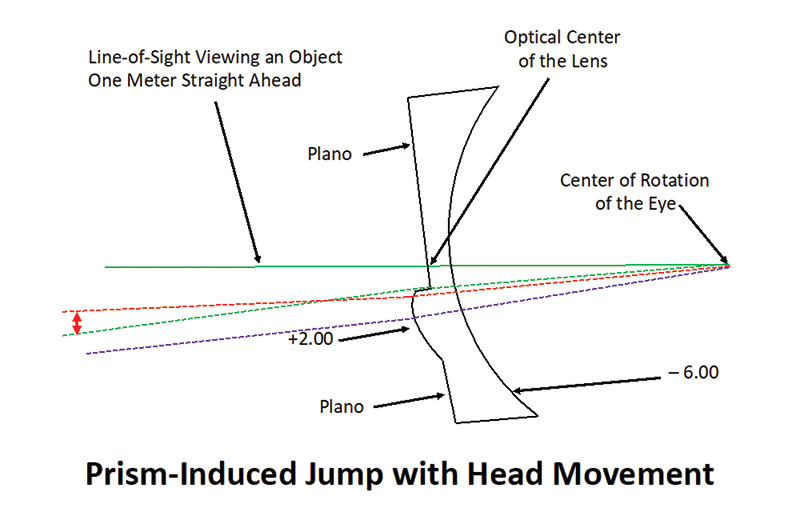
JUMP
Ophthalmic Optics 101 courses always include a discussion of the disconcerting image jump (Fig. 3) that can be found when the line-of-sight passes from the distance portion of a bifocal to the segment. This is perhaps useful in helping students grasp the basics of how prisms work, but it has little practical use in dispensing. When changing fixation downward from a distant object to a near one such as your wristwatch, no jump is observed even though the prism through which you are looking changes suddenly and significantly. This is due to a shutdown of the visual system that occurs when fixation changes.
To demonstrate this, look first at your right eye in a mirror, then at your left, then back again at your right. The movement cannot be seen because our visual system shuts down momentarily as we re-fixate various objects of regard. If you think the movement is just too fast to be perceived, watch someone else try this experiment, and you will see the re-fixation of that person’s eyes is not at all imperceptible.
Image jump in lined lenses is visible with head movement when fixation is held on a single object. The takeaway here is that first time bifocal wearers approaching stairs (particularly descending stairs) should fixate on the stairs through either part of the lens as they approach the challenging stairway, but they should not move their head up or down in an effort to find the appropriate sweet spot. This is an exception to the general rule that newly dispensed patients should be told that each lens has a sweet spot that will tend to enlarge as their eyes respond to the new prescription. Patients should know that when something does not seem clear, they should move their head to find the sweet spots in the lens which will give them a clear view. PAL lens designs do not cause this prismatic jump effect because the power and prism changes are not abrupt. The exception to this would be when a PAL lens includes a slab-off.
DEFINITIONS
1. Optical Center: The point on the optical axis of a lens through which a ray passes undeviated (Fig. 1).2. MRP: The Major Reference Point (MRP) is the point on a lens which gives the exact power and prism specified by the lens prescription. When writing lens prescriptions, it is universally understood the prism is only indicated when needed.
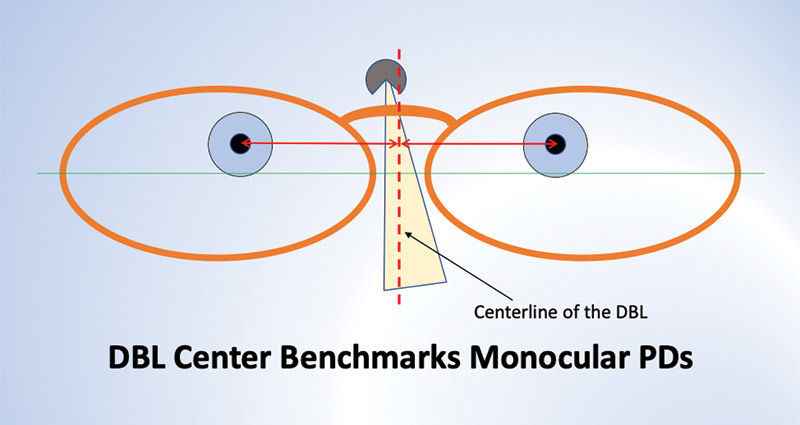
3. Monocular PD: The horizontal distance from the point at which the line-of-sight intersects the lens to a vertical line passing through the middle of the DBL of the fitted frame. In most cases, this is taken with the head tilt in the patient’s preferred position and with the lines-of-sight parallel and level.
4. Major Ray Bundle: The Major Ray Bundle is the ray or ray path represented in object space by the line connecting the point of fixation with the center of the entrance pupil and in image space by the line from the center of the entrance pupil through the center of the exit pupil and connecting with the fovea. This is sometimes also referred to as Foveal Chief Ray.
5. Fitting Cross: The Fitting Cross (FC) is the lens manufacturer’s specified landmark on every PAL around which the other functional points of the lens are located. It is also the point in the lens at which the corridor starts, so for clear, comfortable distance vision, the line-of-sight must pass above the FC.
6. Datum Line: The Datum Line (also called the Mounting Line) is the horizontal line that is halfway between the highest point of the lenses and the lowest point of the lenses when they are measured by the boxing system (Fig. 2).
ANISOMETROPIA
When relatively small amounts of anisometropia are present, it can present challenges of both aniseikonia and ocular torticollis, as well as fusional problems. A patient with an Rx of OD –0.50DS and OS –1.50DS may find they are most comfortable and see best when viewing through a horizontal band a few millimeters wide and centered on the OC of the left lens. In such cases, care should be taken to specify the vertical location of the MRPs when the lenses are ordered. When this patient enters presbyopia, careful binocular testing may reveal that although PALs can be tolerated, he may also be a good candidate for computer lenses for office work and reading.
ADAPTATION
Every ECP has experienced patient complaints which seem baseless when a patient returns shortly after dispensing expressing eyewear related problems although they have 20/20 vision at distance and Jaeger 1 at near. The lenses may have exactly the prescribed powers, and the base curves and thicknesses are appropriate. There may be neither warpage nor apparent waves in either lens. The fit of the frame and cosmetic appearance is not suspect, nor is there any hint of buyer’s remorse other than whatever is affecting performance.
These complaints may arise from the phenomenon of “adaptation,” and a part of adaptation is developing an intuitive ability to move one’s head so the lines-of-sight are better oriented. Patients are often told, “Become a nose-pointer,” and that often works although such advice does little to reassure that their new prescription and lenses are actually correct.
Advising patients at the time of dispensing that their new lenses have sweet spots that will give the best possible performance is a more positive statement. The patient’s task is really to keep looking at whatever is of interest and move their head until they find the sweet spots. Give reassurance that as eyes respond to the new prescription, the sweet spots will enlarge as a normal part of adaptation. This will help avoid and resolve adaptation-based complaints.
Recently, manufacturers have begun offering “variable corridor” PALs in an apparent attempt to avoid the problem of fitting too-long corridors that cut off part or all of the near sweet spot or NRP. As with many other innovations, there are some patient complaints relating to adapting to longer corridors. If a patient is well adapted to a short corridor length, it may not be a good idea to dispense a longer corridor in a new frame with a large B measurement just because you can. On the other hand, advertised minimum fitting heights are sometimes just the distance from the FC to the NRP, and fitting at that height will surely cut off at least the bottom half of the reading area.
For better understanding of sweet spots in lenses, it’s important to remember that for most patients (the ones with binocular vision) there are two sweet spots in every set of single vision lenses you dispense, and for bifocals and trifocals there are more. Sticking to single vision for the moment, there is a right lens sweet spot, a left lens sweet spot, and it is possible that a binocular sweet spot which may play a significant role in adaptation (Figs. 4a and 4b).
FIGURE 4A
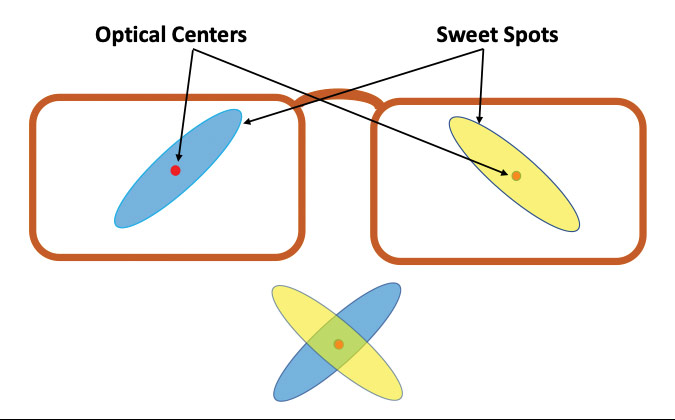
Green spot simulates the limited sweet spot area for binocular vision with non-atoric lenses.
FIGURE 4B
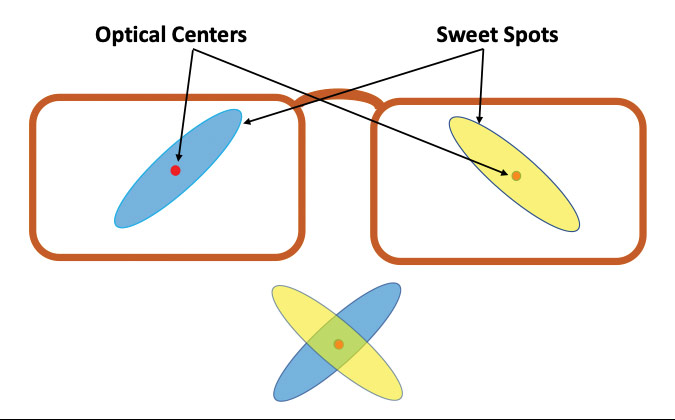
To start with only lens powers and a distance PD, and then design the well performing, comfortable and cosmetically appealing eyewear is a daily challenge for every ECP. To successfully meet those challenges, patience, skill and an understanding of science and human psychology are required. That’s why the very best ophthalmic dispensers are masters of a curious mix of art, science and communication skills.
DESIGN AND DISPENSING TIPS
- Always adjust the frame before taking measurements.
- Use MRP heights for all SV and lined lenses. Keep in mind that exceedingly high or low MRP heights can result in thicker lenses.
- As-worn digital technology is great especially for mid-range and stronger prescriptions and highly sensitive patients, but never use default measurements. Your measurements are likely to be far more accurate than using default values, which are really only shot-in-the-dark averages.
- Stay with a satisfactorily worn corridor length when you can, and place the Fitting Cross location relative to the pupil as it was in the previous eyewear. Even if the B measurement is deeper than with the previous eyewear, keeping its length the same will often allow for easier adaptation and a more satisfactory outcome.
- Variable length corridors seem to be the industries’ attempt to avoid cutting off the lower part of the NRP zone, or near sweet spot. Some patients who have gone to deeper frames with variable length corridors have found the increased down-angle to use the NRP area to be both inefficient and annoying.
- For non-presbyopic patients and first-time presbyopic lens wearers, those who have delayed care and who must start in stronger than average new-adds, recommend using extra light for reading and other near tasks. This has the effect of increasing the depth of field for near work, so the eye-to-object distance is less critical. It also effectively widens the sweet spot for near so less head movement is required for reading, and it widens the corridors, which makes them easier to locate and use
Tootsie Pop is a trademarked product of Tootsie Roll Industries, LLC.