
By Thomas H. Clark O.D.
Parts 1 through 4 of this series described the importance of determining the visual axis measurement to maximize patient visual comfort and satisfaction with PALs. This final installment introduces methods and devices to obtain that measurement.
METHODS AND DEVICES USED TO DETERMINE VISUAL AXES MEASUREMENTS
At the time of these studies, there was no commercially available device or visual system to measure visual axes separation or to verify correct PAL placement. The author developed and produced devices and methods (now patented) to obtain visual axes separation measurements.
Measuring Visual Axes Separation (for fitting point separation)
A reengineered corneal reflective pupillometer was used as the visual axes measuring device (Fig 9). A new target and slit were attached to the digital readout sliders of the pupillometer. As a result, operation, by patients, with their fingers on the sliders has proven to be very convenient and accurate.
This technique of alignment uses a peep sight system similar to peep sights used by Olympic shooters, which are extremely accurate.
As stated, this is an interactive subjective test where the patient moves the slides that the dispenser would usually move in a traditional PD measurement to center the slit borders on a target. The patient maneuvers the pupillometer slides to determine visual axes alignment. When the patient is satisfied with the alignment in both eyes, done monocularly, the dispenser uses the digital readout to determine visual axes separation (Figure 10).

Figure 9. Patient using visual axis device at dispensing table

Figure 10. Patient view of visual axis device with slits
VERIFYING CORRECT SEGMENT PLACEMENT
Measuring progressive lenses and optical positioning when troubleshooting a problem can at times, be a tedious affair. In addition, there are also times when the manufacturer’s markings are too faint to see or appear to be misaligned.
Figure 11 demonstrates a patented method and device, using patient feedback to verify intermediate and reading zone centering. For the first time, this method can determine if the visual axes separation and the finished progressive segments are properly aligned. This device defines any linear error measurement that needs to be corrected when there is a placement error.
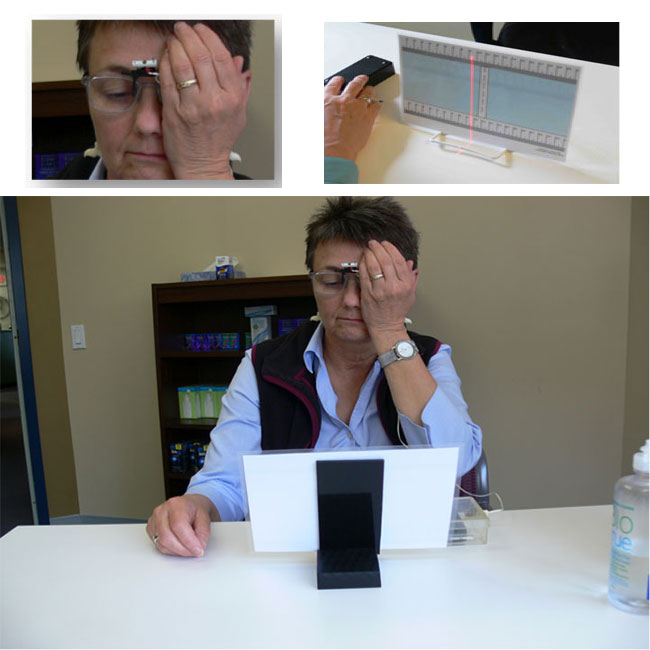
Figure 11. Patient using visual axis verification device at dispensing table
The patient is asked to cover one eye and to scan horizontally to find what position gives the clearest image for a vertical line of letters. This is a surprisingly easy task for the patient because the zones of clear vision and blurred vision are very distinct.
The fixation point on this reading card is noted. Then, the other eye scans for the clearest area while the first eye is covered. That fixation point is noted.
Perfect alignment is when both fixation points are the same.
When alignment points differ, the amount of separation on the near point card can be calculated to determine the alignment error at the patient’s lens plane and can now be corrected, see Figure 12.
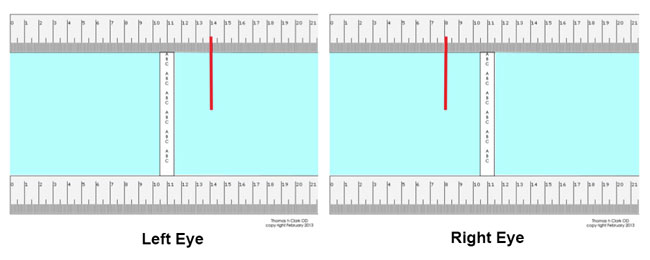
Figure 12. This illustration shows the fixation difference for each eye when viewing the vertical line of letters through the clearest portion of their PAL segs. (a difference of 6cm)
To calculate the linear error of the figure 12 example, note that the difference between the two alignment points (right eye –left eye) at the position of gaze on this chart is 6 cm. Each cm of separation at the reading chart at 16 inches is equal to 0.50mm at the lens plane. The calculation for linear error in this example will be 3.0mm. Remake these lenses with a near segment separation 3.0mm less and you will have a happier patient.
An added bonus of this type of verification device is that a defective lens is easily discovered because a patient will not be able to find an area of clear near vision anywhere in the lens.
SATISFACTION SURVEY RESULTS, 50 PATIENTS
To test the effectiveness of the new device, 50 new patients were sold progressive lenses and asked to answer a survey questionnaire two weeks after receiving their lenses. The results of the survey suggest easier fitting for dispensers and more satisfied progressive lens patients. Compare your impression of the results if your patients were surveyed.
1. How long did it take you to adapt and be comfortable with your new PAL lenses?
42% immediately
23% One day
27% week or less
2. How would you rate your initial comfort when your glasses were dispensed?
67% very good
19% good
3. How many return visits to Dr. Clark’s office were needed to correct visual issues (not frame adjustments)?
79% none
13% One
4. How satisfied are you with the performance of your PAL lenses?
71% - 90 to 100% satisfied
17% - 75 to 89% satisfied
A NEW GOLD STANDARD
Sitting across the dispensing table from an unhappy PAL wearer is not comfortable. Sitting across the dispensing table from an unhappy PAL wearer for the third time is pure hell. In addition, both significantly reduce the ability to be profitable fitting progressives, not to say what that does for overall patient satisfaction and staff morale.
Inaccurate PAL alignment affects each office and the optical industry in general in terms of lost time, income and patients. This author, based on investigation, testing and the development of these prototype instruments believes that there is an opportunity for the use of visual axes measuring instruments to determine more accurate fitting points for the optical dispensing industry. With these measuring devices in place the optical industry will achieve another level of excellence in serving our patient base.
Dr Thomas Clark OD, http://www.willistonoptometrist.com/
For further information on this measuring system contact iPCapital Group.












