By Danielle Crull, ABOM
Augmentative and Alternative Communication devices, also known as AAC devices, are becoming more common for kids who have difficulty communicating. These devices are often used for kids and adults who have no mobility to write and type or are unable to communicate effectively using speech.
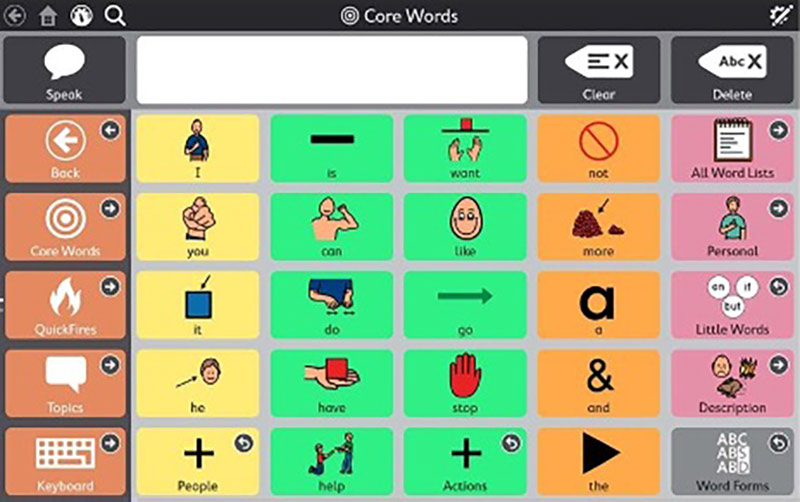
The first known AAC device dates back to 1920. It was called the F. Hall Roe Communication Board. The board contained letters and words that a person would point to in order to communicate words or sentences. I’ve seen similar devices used for the youngest of children in my practice. These boards have pictures of things they may want to communicate. For instance, a cup for “thirsty”, or a toy for “play.” Depending on their ability to move, a child may point on their own or a caregiver may point, and the child communicates a yes or a no. A “yes” might look like an eye blink and a “no” as two eye blinks. Sometimes a child looks to the left for “yes” and to the right for “no.” With the development of iPads and touch screens, the devices themselves can now “say” what the child intends to communicate.
The newest AAC devices employ eye gaze technology. Now the user simply looks at a button on the screen to communicate. With the older point style boards, it would take a lot longer to communicate a complete thought and would be impossible for those who have limited movement. With eye gaze technology, communication is nearly as fast as it is for you and me to communicate.
In my practice, I see more and more kids using these devices. I’ve come to recognize that these kids have unique needs in regard to their glasses fitting and lens choices, which ensures that what we fit them with does not impede the use of their communication technology. Below are a few things to consider:
- Size: It’s important to analyze your patient’s ability to move their head. You’ll find many of these patients are wheelchair users and have restricted head movements. An eye gaze device utilizes a camera or cameras positioned at the bottom of a computer screen. It is important that the size of the frame be large enough not to interfere with the camera's ability to track the user's eye. Frames need to have a larger lens portion below the eye and be wide enough, that as the eye moves, the camera isn’t blocked by the edge of the frame.
- Lens coatings: The camera uses infrared light to track the user's eye movements. It directs infrared light into the eye and calculates the pupil center based on the reflection from the cornea. The use of anti-reflective lenses is beneficial to eliminate glare from either blocking the camera or creating a false additional reflection.
- Pupillary Measurements: Always ask your patient where the device is generally located for them in relation to their eyes. If your patient lies on their side all day long, and the device is above their head, then optical centers and heights need to be adjusted accordingly.
- Lens types: All lens materials seem to work without interference, but some lens types interfere. Lined bifocal or trifocal lenses are the most disruptive. If an add power is indicated, it’s better to fit with a progressive or blended lens. The ridge of the bifocal segment creates a glare line and also adds base up prism, interfering with the camera’s ability to accurately locate the pupil’s center. Polarized filters do not interfere with the camera itself, but a polarization may also be present on the user’s monitor or computer screen. Because of this, polarized lenses may make it difficult for the user to see and locate the buttons they desire to activate. If the patient needs tinted lenses, it’s better to use a tint without polarization.













