ABC's of DCDs
While most eyecare practices continue to be comfortable with and rely upon marker pens, PD sticks, pupilometers and seg-height gauges to obtain the basic fitting measurements for eyewear sales, behind the scenes there has been a quiet revolution. There has been a constant change in the technology of digital imaging and centration devices, or DCDs. Today's DCDs can show customers in their favorite frame choices, demonstrate lens styles and photochromics as well as take all the measurements needed for the most personalized of progressives. Become part of this revolution; it's time. Here's how.
The public's broad acceptance and adoption of tablet-based computing, which includes the Apple iPad and Google Android, along with the latest advancements in processor speed, memory capacity and, particularly, the pixel-depth and resolution of their built-in cameras have made tablets and smartphones the norm. Adding them to your practice allows you to also start enjoying the technological benefits of these advanced electronic aids.
Fast Acquisition of the Basic Measurements
When you end up being really slammed on a busy Saturday, a digital centration device can be a savior. It allows almost any staff member to quickly obtain monocular PDs, pupil heights, pantoscopic tilt, vertex distance and frame wrap in but a few seconds. Add in the assurance of high confidence in the precision and accuracy of the results its like having another employee (well almost). Of course, some training, practice and experience is required to reap the above benefits, but it is certainly not beyond the scope of anyone familiar with the basics of taking measurements by hand (see The Art of Taking Measurements by Hand, etc.) Clients will innately view the use of DCDs as a measure of your commitment to using the latest technology, and the halo effect from employing them in your practice should not be understated.
THE ANATOMY OF DIGITAL CENTRATION DEVICES
The anatomy of these devices is both similar and very different. All have at least one camera (some more than one for three dimensional viewing). Floor standing models have mirrors so the patient, standing in front, can see himself or herself easily centered. The attached monitor images the patient while also providing the menus of capability. Tabletop models can be like floor standing only made for counter or dispensing tabletop. They can also be like a large tablet with a base.
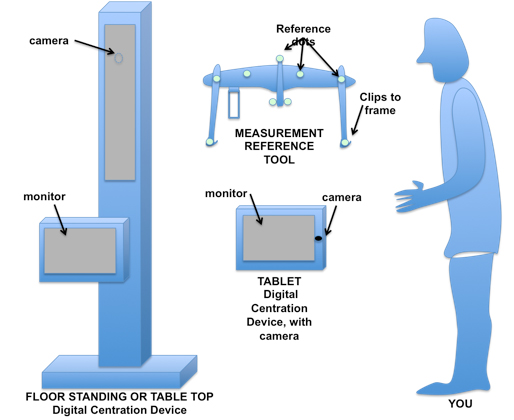
|
Tablets are portable and for many suggest a more modern as well as adaptable approach to the eyewear process. For example, it can travel with the patient and optician, take measurements, pictures and show lens options.
For accurate lens position measurements, a frame reference tool has typically been needed to evaluate tilt, vertex and faceform. In this case, the tool attaches to the frame chosen by the client. Frame reference lines for 'A', 'B' and 'DBL' is adjusted and pupil reflex is 'dotted' electronically. Then, the software for tilt and faceform evaluates the relative position of the reference dots. Some use a prism to determine vertex.
Bottom line, the easier the device is to use, the more complex and sophisticated its inner workings are.
THE ABC'S OF TABLETS
In order to allow the tablet's application software to perform the calculations necessary in deriving the measurements, a fundamental reference is needed. This reference device functions both as a ruler and as a parallax compensator. The type of reference a tablet uses helps to define which of two camps its falls: Those that employ reference devices attached to frames, and those that don't. Both tablet types share common advantages and disadvantages.
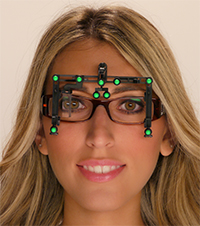
Tablets with a Frame Reference Device
In this group, a lightweight frame reference device (we'll call it the 'FRD') is attached to the wearer's frame. On this FRD are brightly colored or high-contrast cardinal points, which the tablet's software quickly locates and identifies during the process of taking one or more pictures. As the application software is acquiring these cardinal points, it also looks for the corneal reflection, or the circumferential edge of the iris - both areas with characteristically high-contrast.
Although the software is terrific at accurately locating both cardinal and eye points, the application additionally allows for the operator to "tweak" their location manually to enhance precision and ensure the most accurate measurements. Additional guidelines are then presented to the ECP to square up and further fine-tune the position of the bridge and eyewire borders. These guideline adjustments are essential in enabling the software to calculate both monocular PDs and heights.
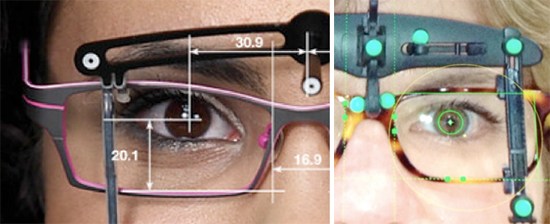
|
|
Frame Reference Device (FRD) |
Tablets Without a Frame Reference Device
Lauded for the unencumbered, open-air feeling the client enjoys, centration tablets without a FRD approach derive the measurement differently. Aligning the tablet's screen format and camera position with the help of its built-in orientation sensor is done in place of attaching an FRD.
This operator-aided alignment provides the cardinal references for the application's software. Because the tablet's proper orientation is essential to the accuracy of the measurement calculations, this approach often use a "go/no-go" signaling guide to help the ECP obtain the best alignment quickly and effectively. As with FRD tablets, manual tweaking adjustments are provided for fine-tuning accuracy. The bridge and eyewire guideline adjustments are done typically by 'grabbing' the line with a stylus and dragging it to the best position. Non-FRD units claim that capturing a client's natural posture is better achieved without the use of attached frame devices.
The Importance of Proper Lighting
Both types of approaches require good lighting for the software to "see" properly. Proper lighting allows for adequate contrast thresholds to be present for capturing the cardinal points. Some tablets include an auxiliary flash attachment to ensure proper illumination thresholds. Other attachments attempt to further enhance camera precision by employing the technique of multiplying pixel depth in the final photo. Regardless, having the right light makes all the difference so consider where and how these tablets will be used.
THE ABC's OF FLOOR STANDING DCDs
With all the inherent convenience of small, hand-held or desktop digital centration units, an ECP might ask if there is any rationale for continuing to consider the purchase of the tablet's big brother: the dedicated, floor standing or desk-mounted DCS. In a word, yes. Larger, formal units often provide a more comprehensive measurement set, which can include the following:
|
|
Optikam |
1. Determination of Head Cape
Head cape is the habitual departure from orthogonally compliant natural posture. For example, when using a Pupilometer, the client is positioned with head and eyes artificially pointed straight ahead. There are no posture effects though that's not the way they would actually wear their glasses.
2. Determination of eye-to-head turn ratios
Some people naturally follow objects or read words by moving their eyes. Others prefer turning their heads. A calculation can be made, expressed as a ratio, to relate the design importance of these two tendencies
3. Evaluation of eye dominance
Most people have a dominant hand, i.e., they are right-handed or left-handed. Similarly, people also favor using one eye over the other, which is often called the person's sighting eye. In lens design, knowing the dominant or leading eye can allow certain software to prioritize acuity for driving or sports in the periphery of the appropriate eye.
An argument can also be made that these larger units provide offer the opportunity for a practice to provide a tiered experience for their clients. For example, everyday lenses can be measured efficiently with tablets, while more expensive, state-of-the-art progressives or single vision lenses could warrant using a more elaborate set-up. Think of it this way: would you like your dentist to take your X-rays with a device about the size of your phone, or a more formal, dedicated piece of equipment?

|

|
|
Essilor Visioffice |
Zeiss I Terminal 2 |
ANY ACHILLES HEEL?
Despite all the wonderful features and convenience inherent in the newest tablet-based DCDs, some obstacles often stand in the way of practice adoption:
1. Increased Time
As with any new tool during the beginning stages of becoming acquainted with its use, the time needed to become proficient is greater. Further, ECPs are often put off by the prospect of appearing clumsy in front of clients. Luckily, the latest's units are extremely easy to use and possess a gentle learning curve.
2. False Benchmarking
Despite the attraction of an expanded measurement set, most ECPs will quickly test a unit under consideration by benchmarking a PD, often their own, against the values of a prospective DCDs.
The problem here is that many offices are unaware of the calibration state of the old pupilometers. Jammed in and out of drawers on a daily basis is not ideal for maintaining a traditional pupilometer's accuracy. Further, most pupilometers are limited to a maximum precision of 0.5mm. Add in even a little mis-calibration, and it is easy to see how a familiar and trusted PD value might actually have been rounded off incorrectly.
Now, with a basic PD measurement incorrectly under suspicion, some ECPs then discount the accuracy of the rest of the measurements, including those they have no experience or familiarity with. This is too bad, and reminds one of the old adage to "not throw out the baby with the bathwater.
3. The importance of Increased Precision
Let's face it: With the current ANSI standards in place, hearing of claims of 0.1mm precision for PDs from the makers of digital centration systems can appear, at least at first blush, as completely unnecessary. But where improved precision and accuracy can really make a difference is in the fitting of mature-add progressives - those 2.25D and over (the majority of adds today).
The intermediate corridors of these adds can average at best 3mm in width. Combine this with a common indoor eye pupil diameter of 3mm, and it's easy to see that fractions of a millimeter can impact overall intermediate binocular utility.
CONCLUSION
A few years ago, the appearance of auto refractors in our offices was accompanied by real trepidation by eyecare professionals. Novel technologies have a way of doing that. First feared by their adopters, in a short time they realize that they have not become obsolete, and just a little while later, the ECP wonders how they ever got along without them. The same scenario is bound to be true for tablet digital centration devices.












