UNRAVELING AMBLYOPIA, STRABISMUS, PHORIAS AND TROPIAS
By Maryann Santos
Release Date: January 1, 2021
Expiration Date: January 1, 2023
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Identify and describe how the eyes' six extraocular muscles move the eye
- Describe and fusion, stereopsis and binocular vision.
- Differentiate between tropia and phoria.
- Provide patients the proper ophthalmic options for the patient.
Credit Statement:
This course has been approved for one (1) hour of Ophthalmic Level II continuing education credit by the ABO. To earn ABO credit, please review the questions and take the test at 2020mag.com/ce. Note: As of January 2020, no tests will be graded manually. Please call (800) 825-4696 for more information.
Amblyopia, strabismus, phoria and tropia are terms we hear occasionally but may not fully understand. This course defines and helps us differentiate between these terms. To understand these eye misalignment conditions and their visual effects, we will first learn about normal eye alignment and image formation in the brain through binocular vision, binocular fusion and stereopsis (3D). You will learn how the eye moves to align images on the retina for clear single vision. Upon completion of this course, you will understand the visual effect of functional vision problems or deficiencies due to incorrect ocular alignment. Lastly, this course provides recommendations for the optician to integrate when working with patients who have functional vision problems or deficiencies.
BINOCULAR VISION, FUSION AND STEREOPSIS
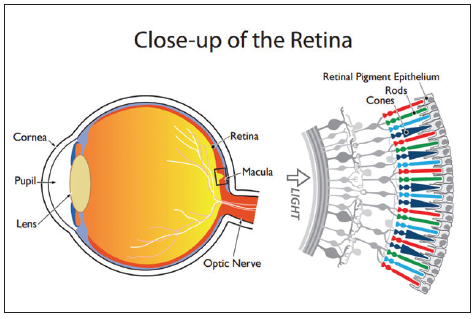
We see with our brain. The retina is an extension of the brain. Images formed on the retina transport to the brain in the form of electrochemical signals via the optic nerve. In order to see a single image, each of our eyes must fixate on the same thing in space and time—this is binocular vision. With good binocular (both eyes) vision, images formed on the retina of each eye overlap in the brain allowing binocular fusion; the brain combines the two overlapping images into one clear image. We need two eyes to produce stereopsis, the ability to see depth in three-dimensional space. To achieve equivalent images on the retinas, the eyes must have normal movement and ability to align the view of objects in our environment. Next, we will learn about the muscles that control eye movement and facilitate proper alignment.
SIX EXTRAOCULAR MUSCLES
The six extraocular muscles originate outside of the globe of the eye and attach to the sclera.
They control eye movement, as we can look up, down, left, right and obliquely. The human eye has four rectus and two oblique extraocular muscles. Listed below are the primary actions of the six muscles. Rectus means straight and oblique means slanted. The rectus muscles attach to the sclera and go back to an area called Annulus of Zinn.
Each muscle has a unique movement. Four rectus muscles do what their name implies: 1. Superior Rectus (SR) moves the eye superiorly (up, elevation). 2. Inferior Rectus (IR) moves the eye inferiorly (down, depression). 3. Lateral Rectus (LR) moves the eye laterally (out toward the temple, abduction), and 4. Medial Rectus (MR) moves the eye medially (in towards the nose, adduction).
Two oblique muscles do the opposite of what their name implies: 1. Superior Oblique (SO) moves the eye down and in (nasally), and intorts (incyclorotation), and 2. Inferior Oblique (IO) moves the eye up, out (temporally), and extorts (excyclorotation).
The goal of the extraocular muscles is to keep the object in view aligned with the fovea of each eye. The retina is the multilayered neuro-sensory tissue that lines the back of the eye. In the center of the retina is the macula, located temporal to the optic nerve. The macula, also known as macula lutea (yellow spot), is responsible for sharp central vision and color vision which enables us to see fine detail and perform visual tasks which require sharp central vision. Located at the center of the macula is the fovea, the area of highest resolution vision. The fovea contains few rod photoreceptors while it is densely packed with cone photoreceptors. This distinction is important because there are two types of photoreceptor cells, cones and rods, but only the cones function for both photopic (daylight) vision and color signals that the brain uses to produce color perception.
Side note: There are three muscles inside the globe—ciliary muscle, iris sphincter and iris dilator. These intrinsic muscles are involuntary and deal with accommodation and the dilation and constriction of the pupil. Now back to the muscles that affect eye movement and alignment.
MUSCLES, TERMS AND MOVEMENTS
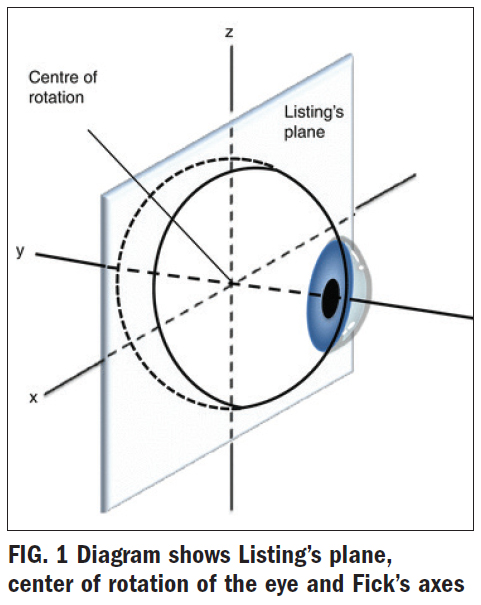
The six extraocular muscles rotate around a theoretical center of rotation. This is referred to as moving around the axes of Fick. There is something called Listing's Plane (Fig. 1), which is like an imaginary plane (picture a sheet of paper) that passes through the rotation center of the eye.
There are three positions of gaze: 1. Primary position looking straight ahead. 2. Secondary position looking up, down, left, right. 3. Tertiary position looking at an angle; either up and out, up and in, down and out, or down and in.
Fick's axes (axes is plural of axis): There are three axes: X is horizontal, Y is sagittal, and Z is vertical. All eye movements can be described as rotations around one or more axes. As a point of reference, the axes intersect at the center of rotation, a fixed point, 13.5 mm behind the cornea.
X, Y and Z axes of Fick's: 1. X-axis—horizontal (transverse divides into top and bottom) axis that runs from nasal to temporal. 2. Y-axis—sagittal (divides into left and right) axis running from the anterior pole to the posterior pole, and 3. Z-axis—vertical axis that runs from superior to inferior.
Find the X-axis in Fig. 1. Elevation and depression of the globe occur around the X-axis. Now, locate the Y-axis. The Y-axis goes through the pupil and runs anterior to posterior. Torsion movements occur around the Y-axis. Torsion movements are those where there is a rotation of the globe, both nasally (incyclotorsion) and temporally (excyclotorsion). Picture a bicycle wheel on the eye with a big red star at the 12 o'clock position. Look at the imaginary red star, and when the wheel turns toward the nose/ nasally, this is called an intorsion. Now picture the wheel turning temporally/toward the ear, this is called an extorsion (not to be confused with extortion!). And last but not least, locate the Z-axis which runs through the eye vertically. Medial and lateral movements occur around this axis. Medial and lateral movements are those when looking side to side, in the direction of the ear or the nose, shifting the eyes right and or left. Refer back to Fig. 1 to see which extraocular muscles rotate around which axes.
MONOCULAR MOVEMENTS OF THE EYE
Ductions are movements involving one eye. Ductions describe monocular movements toward or away from the centerline of the body. For our purpose, we use the nose as a point of reference. Movements will be described as rotating around either the X, Y or Z-axis.
Rotations around the vertical, Z-axis:
- Adduction—moves the anterior pole medially/ towards the nose
- Abduction—moves the anterior pole laterally/ towards the ears
- Elevation—moves the anterior pole up
- Depression—moves the anterior pole down.
- Intorsion – rotation nasally
- Extorsion – rotation temporally
AXES OF THE EYE
- Visual axis: The line that passes from the fovea to the point of fixation (object of regard). The normal visual axes (from both eyes) intersects at the point of fixation.
- Optical axis: It is the line extending from the anterior to the posterior pole of the eye and is defined by the geometric centers of the crystalline lens and the cornea.
- Fixation axis: It is the line joining the fixation point and the center of rotation.
Angle kappa is the angle between visual (optical) axis and the anatomical (pupillary) axis.
The fovea lies just temporal to the anatomical axis. A light shown into the cornea will create a corneal reflex (on the visual axis) just nasal to the center of the cornea in both eyes (positive angle kappa = 5 degrees).
Adduction and abduction are opposites. Their names can be confusing, as there is a one letter difference with the letters themselves (b and d) looking similar. Both refer to movement, in our case, rotation of the eye toward or away from the centerline. Abduction means away. An easy way to remember is by this: The kitty was abducted (taken away) from the yard. The example has a happy ending as the kitty was safely returned moments after.
Adduction is toward the centerline, medially or toward the nose. These terms are important when describing a permanent or occasionally turn or drift of the eyes.
BINOCULAR MOVEMENTS OF THE EYES: VERGENCE AND VERSIONS
Vergence refers to the movements of two eyes in opposite directions. Two terms associated with this are convergence and divergence. Convergence is when both eyes turn in. The eyes converge to read. When converged, both eyes are adducted. Conversely, divergence is when both eyes are abducted; both eyes are abducted as they move out from the centerline.
Versions are when the eyes move in the same direction. Take a moment to look right. Both eyes move to the right. Your right eye turns temporally, while your left eye turns nasally. Dextroversion—right gaze (remember OD stands for Oculus Dexter, right eye); Laevoversion—left gaze (ancient Greek word for "on the left side"); Supraversion—both eyes elevated (above, as in the Toyota Supra); and Infraversion— both eyes are depressed (from the Latin meaning below).
Elevations: Movements of the eyes up and to the right = dextroelevation; up and to the left = laevoelevation; down and to the right = dextrodepression; and down and to the left = laevodepression. These versions bring the eye into the tertiary positions of gaze.
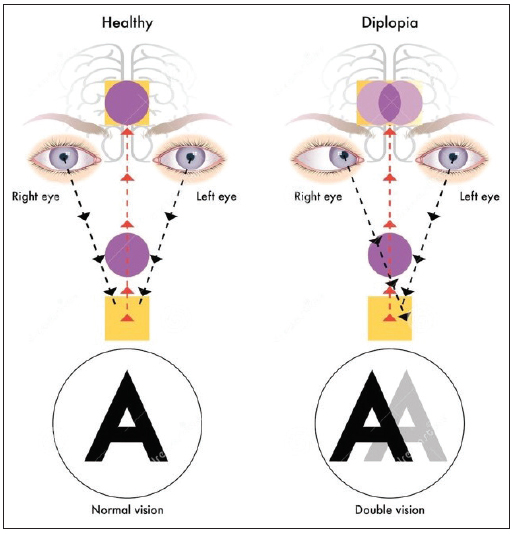
Binocular vision is the ability to maintain visual focus on an object with both eyes, creating a single visual image. It is commonly said that vision takes place in the brain; the retina is an extension of the brain. Binocularity is when two separate retinal images are fused into one by the brain. Disorders of binocular vision can produce diplopia (double vision) a symptom of conditions such as strabismus, convergence insufficiency and aniseikonia. The brain can eliminate double vision by ignoring all or part of the image of one of the eyes; this is referred to as suppression. Binocular vision is also referred to as fusion or binocular fusion.
Fusion is the power exerted by both eyes to keep the position of the eyes aligned so that both fovea's project to the same point in space. Recall from earlier that the fovea (fovea centralis) is in the center of the macula where visual acuity is the highest and is responsible for sharp central vision. Fusion is the perceptual blending of two similar images, one from each eye, into one image that is maintained as the eyes converge or diverge. Fusion is also referred to as binocular vision.
Stereopsis depends on accurate correct alignment of both eyes on the same object. Stereopsis allows one to judge the distance between themselves and objects. An example of depth perception is the ability to accurately judge distances such as when we reach for a cup of coffee or walk up or down stairs. Good binocular vision and fusion is essential for stereopsis.
Try this experiment to see how your eyes see three dimensionally (3D). Hold up one index finger directly in front of you at about arm's length. Your finger is the point of fixation. As you stare at your index finger, your fovea's (fovea centralis) are in alignment on this point of fixation. Stare at your finger and cover or close your right eye. Notice how your finger shifts to the right. If you have an object in the background, this phenomenon will be more dramatic. With both eyes open, fixating on the index finger, the brain blends the images of the two eyes into one at the visual cortex. The visual cortex is the part of the brain where visual processing occurs. Adult eyes are separated by approximately 63 millimeters. Because the two eyes are viewing objects from two separate positions and angles, there are differences in the positions of the images projected onto the retina as demonstrated in the index finger example above. This is called retinal disparity. Retinal disparity is a visual cue used by the brain to determine depth.
Suppression is a phenomenon often seen in strabismus (see below) patients. Suppression is where one eye (retinal fovea) has complete dominance over the other eye and suppresses (ignores) the input from the fellow eye. The human body is designed this way to prevent asthenopia (commonly known as eyestrain/eye fatigue) and diplopia (double vision) by suppressing the image from one eye. The suppressed eye is typically the deviated eye.
PHORIA AND TROPIA
Andrea P. Thau, OD states, "A tropia is a deviation of an eye from the normal position when both eyes are open. A tropia does not always have to be present. There are intermittent tropias, which are only present some of the time. The definition of a phoria is a deviation of the eyes from alignment when fusion is broken (one eye is covered)." During the eye examination, phorias are detected by breaking fusion. Fusion keeps the eyes straight. The practitioner can break fusion and bring out a phoria by performing a Cross-Cover Test, also called an Alternating Cover Test.
During the eye exam, the doctor breaks fusion or binocular vision by occluding one eye. They are not allowing the eyes to "talk" to each other. A phoria is a latent tendency of the eyes to deviate. Fusion or binocular vision prevents the deviation; the phoria is only evident when an occluded eye is uncovered. The doctor will use the Alternating Cover test to identify a phoria. An eye with a phoria will straighten when uncovered. Recall, if it is a phoria, deviations can be noted by the direction of the eye turn: esophoria, exophoria, hyperphoria or a hypophoria (in, out, up, down). Treatment can be in the form of prescription eyewear with or without prismatic correction and through optometric vision therapy.
Tropia comes from the word tropism, or nonpareil (unrivaled) in biology. Tropism is a turning, of all or part of, an organism in response to an environmental stimulus. Tropias are detected during the eye examination with the Cover/Uncover test.
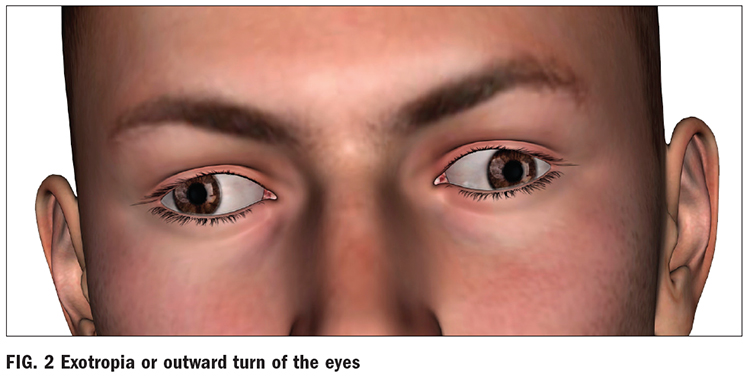
Treatment can be in the form of prescription eyeglasses, patching one of the eyes, surgery to either shortening or lengthening the rectus muscles, or by optometric vision therapy. Recall, if the patient has a tropia, deviations are noted in the direction of the eye's position: esotropia, exotropia, hypertropia, or a hypotropia (in, out, up, down).
COVER/UNCOVER TEST AND ALTERNATE COVER TEST
As mentioned above, there are two types of Cover test, the Alternate Cover test and the Cover/Uncover test. These tests determine if the both foveas of each eye are maintained on the target.
A Cover/Uncover is performed with the patient looking through their habitual prescription. The patient looks straight ahead and the eye doctor covers one eye with an occluder. The examining doctor carefully watches the uncovered eye for any movement. The presence of movement by the uncovered eye indicates a heterotropia. If the uncovered eye does not move, the eyes are in alignment i.e. orthotropic. If an eye is turned in, it is called esotropia. If the eye is turned out, it is called exotropia. If the eye is turned up, it is called hypertropia and if the eye is turned down, it is called hypotropia. For example, if someone has esotropia in their right eye, the eye would have to turn out to pick up fixation. That deviation indicates an esotropia.
The Alternate Cover test is similar in that the patient is looking straight ahead and the examining doctor also uses an occluder. The difference is that fusion is being broken. The examining doctor will move the occluder from the left eye to right eye and left eye to right eye, back and forth. This breaks fusion. The examiner can detect a deviation once fusion is broken. If the Cover/Uncover test determines the absence of a tropia in either eye, the Alternate Cover test is then performed to check to see if there is a phoria.
Ideally, the eyes work together binocularly; each eye forms an image on the retina of the same object in space and time. With good binocular vision, the brain fuses the two images together to form one clear image. When the eyes are properly aligned the eyes look and point in the same direction when looking at an object. When there is a misalignment, strabismus may be detected. When the eyes are misaligned, the individual may have strabismus, which is known as a squint. In this article, ocular misalignment will be referred to as strabismus. Deviations can be: EXO meaning outward (Fig. 2), ESO meaning inward, HYPER meaning upward and HYPO meaning downward.
Strabismus is when there is a misalignment of the eyes. One of the main symptoms of strabismus is an obvious visible misalignment of the eyes; one of the eyes does not appear to be looking straight ahead. The misalignment is measured in angles of deviation and can vary from very small to large. According to the American Academy of Ophthalmology, approximately, 4 percent of children in the United States live with strabismus. Strabismus can be treated by eyeglasses, eyeglasses with prism, vision therapy or eye muscle surgery.
- A condition in which both eyes do not look at the same place at the same time.
- Can occur when an eye turns in, out, up or down due to poor eye muscle control.
- Two different (disparate) images are sent to the brain—one from each eye. The brain is unable to fuse the two disparate images into one clear image.
- Congenital—condition is present at or shortly after birth.
AMBLYOPIA (LAZY EYE)
Andrea P. Thau, OD, informs us that amblyopia is a failure of the eye to develop clear vision. Amblyopia (lazy eye) has several etiologies. It can be caused by uncorrected unilateral or bilateral refractive error. Large uncorrected refractive errors in both eyes or unequal refractive errors (anisometropia) may deprive the retina of a clear image and lead to a failure to develop good visual acuity. Amblyopia can also be caused by a strabismus or visual deprivation from birth such as a cataract, ptosis (drooping or sagging of the upper lid), or corneal opacities. In children, the brain may learn to ignore the image from the amblyopic eye which leads to depth perception problems. In adulthood, strabismus is referred to as acquired. This is typically caused by injury to the eye orbit or injuries to the brain, such as with a stroke or head injury—acquired strabismus results in double vision (diplopia).
Symptoms are subtle and often detected by the parents that notice the child squinting, tilting, or turning their heads to see better by covering an eye to see better. When one eye sees better than the other, the brain ignores the other image. The strong eye gets stronger while the weaker eye gets weaker. Strabismus, as noted above, along with uncorrected refractive errors, can result in amblyopia. Refractive amblyopia is when the brain is seeing out of the stronger eye, and the weaker eye's vision does not develop. Myopia, hyperopia, and astigmatism are only detected during a vision examination. An example of this is anisometropia, where the eyes have significant unequal refractive errors. Example: Right Eye +6.25-2.00 X 170 with Left Eye +1.25-0.50 X 165. The eye with the larger error does not develop fully normal visual acuity. Amblyopia can be treated by prescribing glasses or contact lenses and patching the stronger eye, which forces the patient to use the weaker eye. This treatment requires commitment from the child and the family. If left untreated, amblyopia can result in potentially permanent vision loss and problems with depth perception. This is a result of the brain ignoring the images of the weaker eye avoiding double vision. Early detection is vital to avoid vision loss and depth perception issues. Young children typically cannot communicate that their world is blurry.
Dr. Thau invites us to visit the American Optometric Association’s Pediatric Clinical Practice Guideline AOA Pediatric Clinical Practice Guideline and the AOA website to learn more on this important topic.
IN THE DISPENSARY
Amblyopia, strabismus, tropias and phorias are detected during optometric and ophthalmologic examination by various measures such as, but not limited to, the refraction, cover/uncover test, alternating cover text, Maddox Rod, Hirschberg Test and a comprehensive in-person eye examination.
LENS SELECTION
The examining doctor will work with the optician to prescribe the ophthalmic lenses that will work best for the patient. It can be in the form of single vision, lined bifocal, or a progressive lens that may include prismatic lenses. When a patient is prescribed prism in their eyeglasses, ask the examining doctor afterward why and how the prescription was determined. These conversations will help build your knowledge base. You may learn that a patient presented with a head tilt that was confirmed by viewing the driver's license picture along with asthenopia. You may learn that the patient was experiencing diplopia.
UNDERSTANDING VISION THERAPY
One way of managing ocular deviations is with optometric vision therapy. Optometric vision therapy is a non-surgical way of improving visual performance and perception by working with the eyes and the brain. There is a variety of methods used by optometrists to improve amblyopia, strabismus, diplopia, convergence insufficiency, etc. Part of the care can include prescription eyeglasses, contact lenses, prismatic lenses, filters and lens tints. Other methods may also include patches, computerized programs, balance boards and sensory training devices. The program of care typically includes both in-office and at-home eye-brain exercises, which can help improve visual acuity, fusion, stereopsis and visual performance.
CONCLUSION
I hope this course has broadened your understanding of the ocular muscles and positions of gaze of the human eye. Correction or treatment for the aforementioned anomalies can be in the form of prescription eyeglasses with or without prism, contact lenses for distance or multifocal, orthokeratology/ortho-k (corneal reshaping of the cornea with contact lenses to improve vision) or optometric vision therapy. An area not to overlook is advocacy. Opticians have a unique opportunity to advocate for early childhood in-person comprehensive eye examinations. This can be a marketing effort for your practice, through local boards of education, or as a part of state society or civic work such as the Lions Club. State optometric and ophthalmology associations may be able to provide assistance to help promote annual in-person eye examinations in the community.