NEUROLENS: A BREAKTHROUGH SOLUTION FOR HEADACHES, NECK TENSION AND DIGITAL EYESTRAIN
A Systematic Approach to Meaningful Outcomes
By Jeff Hopkins
Release Date: May 1, 2020
Expiration Date: May 1, 2022
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Understand the relationship between digital eyestrain and the ocular motor imbalances that lead to visually induced trigeminal dysphoria.
- Understand the neurolens measurement and treatment solution that measures and identifies misalignment in the visual tracking system and corrects it via a contoured prism lens design.
- Understand the practice building implications of delivering relief for the myriad of CVS sufferers.
Faculty/Editorial Board:
Jeff Hopkins
Credit Statement:
This course has been approved for one (1) hour of Ophthalmic Level II continuing education credit by the ABO. To earn ABO credit, please review the questions and take the test at 2020mag.com/ce.
NOTE: As of January 2020, no tests will be graded manually. Please call (800) 825-4696 for more information.
INTRODUCTION
 Digital eyestrain, also known as computer vision
syndrome, is one of the most widespread vision-related problems we face today. According to a
2016 report by The Vision Council, Americans
spend an average of nine hours per day using a
digital device, and 70 percent use two or more
devices at the same time. Sixty-five percent of
American adults suffer from one or more symptoms of digital eyestrain daily. Based on data collected from over 50,000 eye exams, 57 percent of
patients suffered from three or more symptoms.
The most common symptoms were tired eyes (54
percent) followed by neck pain (51 percent), discomfort while using a computer (41 percent), dry
eyes (39 percent) and headaches (36 percent).
Digital eyestrain, also known as computer vision
syndrome, is one of the most widespread vision-related problems we face today. According to a
2016 report by The Vision Council, Americans
spend an average of nine hours per day using a
digital device, and 70 percent use two or more
devices at the same time. Sixty-five percent of
American adults suffer from one or more symptoms of digital eyestrain daily. Based on data collected from over 50,000 eye exams, 57 percent of
patients suffered from three or more symptoms.
The most common symptoms were tired eyes (54
percent) followed by neck pain (51 percent), discomfort while using a computer (41 percent), dry
eyes (39 percent) and headaches (36 percent).
It is clear from this list that there is a whole complex of symptoms that fall under the category of digital eyestrain, and to treat them, a complex of solutions are currently available. Some of these take the form of lens designs, such as “computer lenses” that offer an expanded intermediate area for viewing a computer monitor, but typically have no distance vision for the presbyope. For the single vision lens wearer, lenses with a small boost of add power in the lower portion of the lens make it easier to view handheld digital screens. A range of lens monomers and coatings reduce the wearer’s exposure to high-energy blue light from screens. Short-wavelength blue light from screens is difficult for the eye to focus due to its intrinsically myopic (defocused) nature.
For this reason, blue light may contribute to digital eyestrain. Behavioral changes are also frequently recommended to patients, such as better posture at the workstation and the 20-20-20 rule (every 20 minutes look 20 feet away for 20 seconds). But these treatment options only address the outward symptoms of digital eyestrain. What has been lacking is an understanding of the root cause and a means of directly addressing the root cause.
New research has revealed that the root cause lies with the interaction between the eyes and the brain. Referred to as visually-induced trigeminal dysphoria, it stems from the overstimulation of one of the key nerves in the brain. Dysphoria is defined as a profound sense of unease or dissatisfaction; it derives from the Greek word dysphoro, meaning “difficult to bear.” Trigeminal dysphoria can cause headaches, eyestrain, dry eye, neck pain and shoulder pain, all common symptoms of digital eyestrain.
In this course, we will look at the relationship between digital device use, trigeminal dysphoria and the visual phenomena that cause it. Most importantly, for eyecare professionals and their patients, we will look at new technology from Neurolens, Inc., for detecting the causes of trigeminal dysphoria and a new type of eyeglass lens—the neurolens—that can alleviate the symptoms, thereby reducing the symptomatic effects of digital eyestrain.
THE TRIGEMINAL NERVE
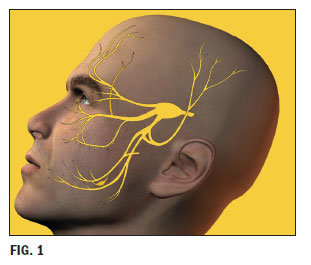 The trigeminal nerve is the most complex
nerve in the cranium. It is responsible for
sensation in the face, as well as for functions
like biting and chewing. It has three branches: the ophthalmic nerve, the maxillary
nerve and the mandibular nerve (Fig. 1). It’s
the ophthalmic nerve that is of interest to us
here. This nerve transmits sensory information from the visual system to the central
nervous system. The ophthalmic branch can
become irritated by overstimulation. This in
turn causes dilation of blood vessels near or
on the surface of the brain, leading to headaches. The trigeminal nucleus extends all
the way to the top of the spine, which means
that irritation can cause neck and shoulder
pain as well.
The trigeminal nerve is the most complex
nerve in the cranium. It is responsible for
sensation in the face, as well as for functions
like biting and chewing. It has three branches: the ophthalmic nerve, the maxillary
nerve and the mandibular nerve (Fig. 1). It’s
the ophthalmic nerve that is of interest to us
here. This nerve transmits sensory information from the visual system to the central
nervous system. The ophthalmic branch can
become irritated by overstimulation. This in
turn causes dilation of blood vessels near or
on the surface of the brain, leading to headaches. The trigeminal nucleus extends all
the way to the top of the spine, which means
that irritation can cause neck and shoulder
pain as well.
Some typical triggers for this irritation appear to be too much caffeine (or too little), drinking alcohol in excess, hormonal changes, certain types of medication and even weather changes. Common visual triggers for trigeminal dysphoria can include bright lights, fluorescent lights and TV and movie viewing. It is believed that migraine headaches can be the result of an oversensitive trigeminal nerve.
Research suggests that digital eyestrain is a form of visually induced trigeminal dysphoria resulting from an overstimulation of the ophthalmic branch of the trigeminal nerve as a result of near work, particularly the use of digital devices. However, despite the recent predominance of digital devices, these symptoms are not new. Optometric literature reveals complaints of similar symptoms throughout history, predating the use of digital devices. In the 1800s, similar symptoms were reported from those who did needlework, for example.
CAUSES OF TRIGEMINAL DYSPHORIA
Visual induced trigeminal dysphoria is a term that describes the constellation of symptoms commonly experienced by many patients. The symptoms of trigeminal dysphoria include headaches, eyestrain, dry eye sensation, neck and shoulder pain. New research has revealed insight into the interaction of the eyes, the brain and the resultant symptomology. Dysphoria is defined as a profound sense of unease or dissatisfaction, from a Greek term meaning “difficult to bear.” It is this unease (or dysphoria) that has lead researchers to link these interrelated symptomologies of headaches, eyestrain, dry eye sensation and neck-shoulder pain back to the incredibly complex trigeminal nerve system.
Proprioception is defined as the perception of body position and movements of the body. If you close your eyes and keep your eyes closed, you will still be aware of your eye movements if you gaze from left to right. This is the proprioceptive feedback loop or sometimes referred to as a sixth sense. In the same sense, if you move your hand in front of your face or hold your hand in front of your closed eyes, you are still aware of that hand position, this is also a form of proprioception. There is a direct proprioception feedback loop from the extraocular muscles back to the ophthalmic branch of the trigeminal nerve. In trigeminal dysphoria, it is believed that this “over-stimulation” from the proprioceptive feedback loop may be the main contributing cause of the various symptomology.
A comparable example is if you drink an ice-cold drink too fast, the result may be “brain freeze” or a sharp headache. The rapid temperature change excites a neural feedback loop back to the trigeminal nerve and causes this pain sensation. Overstimulation of the ophthalmic branch of the trigeminal nerve can result in pain, headaches, eyestrain, dry eye symptoms and head/neck pain.
In the case of the extraocular muscles, the proprioceptive function continually provides vital information on the position of the eyes to help the brain form and maintain a binocular image.
EXTRAOCULAR MUSCLES
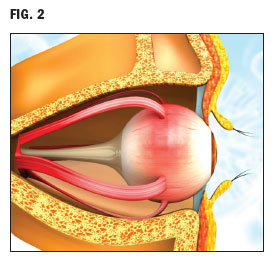 “There are six muscles, which are responsible for controlling the movement of the
eyeballs. They are extrinsic eye muscles
meaning that they originate outside of the
eyes’ orbit. They attach to the outer surface
of the Sclera (Fig. 2). The extrinsic eye
muscles are some of the fastest contracting
and most precisely controlled skeletal muscles in the human body and function as
agonist and antagonist pairs to move the eyeball: 1. Superior and Inferior Rectus muscles. 2. Lateral and Medial Rectus muscles,
and 3. Superior and Inferior Oblique muscle.
“There are six muscles, which are responsible for controlling the movement of the
eyeballs. They are extrinsic eye muscles
meaning that they originate outside of the
eyes’ orbit. They attach to the outer surface
of the Sclera (Fig. 2). The extrinsic eye
muscles are some of the fastest contracting
and most precisely controlled skeletal muscles in the human body and function as
agonist and antagonist pairs to move the eyeball: 1. Superior and Inferior Rectus muscles. 2. Lateral and Medial Rectus muscles,
and 3. Superior and Inferior Oblique muscle.
“The Rectus muscles are primarily responsible for the movement of the eyeballs in the four cardinal directions: up, down, left and right. The pair of Oblique muscles are responsible for controlling the adjustments involved in counteracting head movements, in other words being able to keep your focus on something whilst your head move.” (musclesused.com)
Our visual system entails a complex relationship of fast (saccadic) and slow (pursuit) eye movements and coordination of both eyes (binocularity) to create a seamless view of the world. Our modern world has placed extensive increased near demands with the increased use of computers and mobile devices. Now more than ever before, there is the need to create the most “comfortable” vision and not just clear vision. If there is a mismatch or imbalance between the proprioceptive feedback loop/trigeminal nerve and our eyes, the result is over-stimulation. Small amounts of misalignment or overstimulation of the proprioceptive system can result in dysphoria or overactivity of the trigeminal nerve (Fig. 1). By reducing overstimulation, even small amounts, the result could be greatly reduced symptoms.
Example of trigeminal overstimulation: Brain freeze happens when something cold hits the roof of your mouth, where it triggers your trigeminal nerve. It’s the nerve in charge of sensations you feel around the front of your head, hence “brain freeze or pain.”
The results of trigeminal dysphoria are some of the most common symptoms of digital eyestrain, including headache, neck and shoulder pain, and eye irritation that feels to the patient like dry eye, even if no evidence of actual dry eye is present.
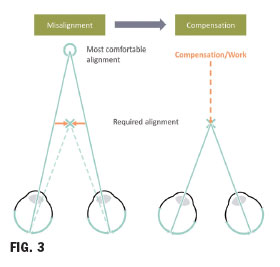
The degree of misalignment that we are discussing here is far more subtle than is the case with strabismus. It will often go unnoticed because it doesn’t cause a loss of binocularity. However, it places a high demand on the visual system to compensate for the misalignment in order to maintain good binocular vision.
There are several reasons, then, why the link between a misalignment in the vision system and the symptoms of digital eyestrain has not been understood until recently. First, the symptoms of this condition are not a loss of binocularity, but symptoms that a patient might not directly relate to their vision. Second, up until now, there hasn’t been an effective way of detecting this subtle type of misalignment, and third, there hasn’t been an effective way of treating it.
 DETECTING MISALIGNMENT:
THE NEUROLENS
MEASUREMENT DEVICE
DETECTING MISALIGNMENT:
THE NEUROLENS
MEASUREMENT DEVICE
An understanding of the root cause that is creating the symptoms of digital eyestrain represents a breakthrough in itself. But this is only good news for the patient to the extent that we can detect and measure the presence of the misalignment that causes trigeminal dysphoria and provide a solution that directly addresses the causes of trigeminal dysphoria. Fortunately, the neurolens Measurement Device provides both.
Let’s start with detection and measurement. Various instruments and tools have been used in the past to assess binocular alignment issues. Still, they have been subjective, relying on conscious feedback from the patient and to varying extents, time consuming and inconsistent in results. The innovative neurolens Measurement Device changes all of that, providing a truly objective and highly precise measurement, even of small otherwise undetectable misalignments in the visual system. It does this by isolating peripheral and central vision to provide a comprehensive assessment of the patient’s eye alignment and synchronization.
 The neurolens Measurement Device (Fig. 4)
measures all of the elements that are critical
for binocular fusion including:
The neurolens Measurement Device (Fig. 4)
measures all of the elements that are critical
for binocular fusion including:
- Pupillary distance
- Heterophoria (a condition wherein the two eyes, while at rest, are not pointing in the same direction when not engaged in binocular fusion)
- Accommodative converge to accommodation ratio (the total amount of accommodative convergence a patient undertakes for each diopter of accommodation)
- Alignment of binocular peripheral and central fusion
- Central fixation disparity (a small misalignment of the eyes when viewing with binocular vision)
First, the neurolens Measurement Device measures pupillary distance. This is done by presenting a fusible visual stimulus (i.e., one that can be focused on with binocular vision) at a simulated distance of 6 meters. With the eyes thus relaxed, the center of each pupil is identified, and the distance between them is measured.
Next, the patient is tested for heterophoria. This is done by showing each eye a stimulus that cannot be fused into a binocular image. Each eye is then shown both peripheral and central fixation targets positioned to align with the patient’s phoria. The targets are slowly moved to induce an 8 diopter divergence. The maneuver is performed to relax the extraocular muscles and neutralize the tendency of the eyes to accommodate and converge when looking into a testing device.
After this relaxation exercise, the patient is shown rotating spheres of stars and planets in the mid-periphery of both the right and left eye simultaneously (Fig. 5). These rotating spheres stimulate the peripheral visual tracking system. While the spheres continue to rotate simultaneously in the mid-periphery of both eyes, a small central target activating the central tracking system is shown to both eyes in the center of the rotating spheres. This central stimulus is shown with alternating occlusion, that is. First, one eye is covered and then the other.
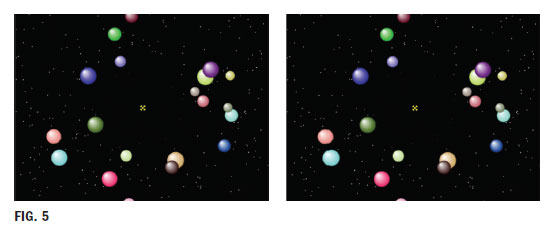
If there is no imbalance between the patient’s central fixation and peripheral tracking system, the dot appears stationary. If there is an imbalance or disparity between central fixation and the patient’s peripheral tracking system, the dot seems to dance with as one eye and then the other is covered, as the two eyes see the central dot in two different locations. Misalignment of central and peripheral vision is then measured in diopters using eye-tracking. The fixation disparity is then neutralized through the use of a prism, and the patient sees the dot as stationary even as the eyes continue to be covered alternatingly. The complete testing process is then repeated for near vision at a distance of 50 cm.
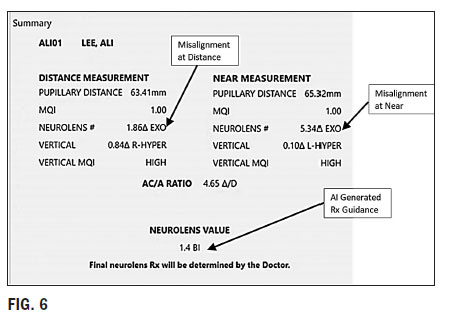
The device collects nearly 10,000 data points to characterize the patient’s eye misalignment, which not only includes typical measurements such as heterophoria and fixation disparity, but other novel measurements such as how fast a patient’s eyes reach a phoric posture, and what a patient’s residual fixation disparity is when fused at their phoric posture. With an average test time of three minutes, the device summarizes all the data into a precise eye alignment measurement for distance and near. The neurolens Measurement Device yields a simple prescribing guideline from its database of symptoms, measurements, treatments and outcomes. In this way, the neurolens Measurement Device allows the eye doctor to leverage the latest technologies, such as eye-tracking, stereoscopic display, machine learning and artificial intelligence, to assist them in prescribing the proper treatment to alleviate the patient’s symptoms.
THE INVENTION OF CONTOURED PRISM
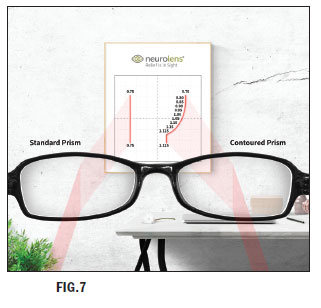 The method of correcting misalignments
has always been prism, and that is the case
here. What is different and innovative in the
case of neurolenses is the accuracy of the
prism and its unique design. In the past, it
has only been possible to create a lens with
one prism power throughout the entire lens.
However, research has shown that 90 percent of patients with trigeminal dysphoria
have a larger misalignment at near than at
distance and therefore need more prism for
near vision.
The method of correcting misalignments
has always been prism, and that is the case
here. What is different and innovative in the
case of neurolenses is the accuracy of the
prism and its unique design. In the past, it
has only been possible to create a lens with
one prism power throughout the entire lens.
However, research has shown that 90 percent of patients with trigeminal dysphoria
have a larger misalignment at near than at
distance and therefore need more prism for
near vision.
For the first time, neurolens addresses this problem with a contoured prism; that is, a prism that changes power from the top to the bottom of the lens based on the patient’s differing needs at distance and near (Fig. 7). For example, the patient might only need a small amount of prism, like 0.25 diopters, at distance, but over one diopter at near. The neurolens design assures a smooth transition and continual eye alignment at all distances. The difference between the contoured prism and a traditional prism is analogous to the difference between a progressive lens and a single-vision lens.
A contoured prism is only possible through digital freeform lens manufacturing technology. Instead of traditional lap tools, which can only put a simple spherical or cylindrical curve on a lens, freeform’s single-point multi-axes cutting tool can put virtually any curve, no matter how complex, on the lens with greater precision than has ever been possible before. Neurolenses are available in progressive, single vision and computer lenses. Apart from the task-specific computer design, they will provide clear, comfortable vision for all activities, all day long.
HOW WELL DOES IT WORK?
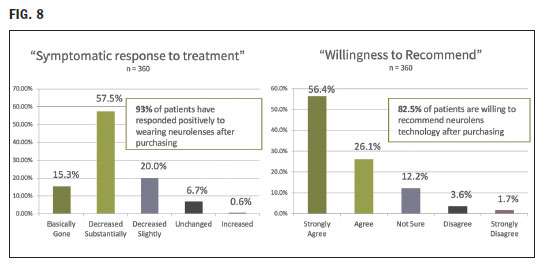
An impressive amount of research has led to understanding the vision issues that lead to trigeminal dysphoria, the development of the neurolens Measurement Device and the design of neurolenses themselves. But none of that would matter if neurolenses didn’t achieve the desired result: relief from the symptoms of digital eyestrain. Two studies bear out the effectiveness of neurolenses for digital eyestrain sufferers and others.
One study conducted in 2012 and 2013 used a prototype neurolens Measurement Device for a study of patients suffering from refractory Chronic Daily Headache; that is, patients with daily or near-daily headaches that have been unresponsive to traditional treatments. These patients initially reported the severity of their pain using a standard test. They were then tested using the neurolens Measurement Device and fitted with neuro-lenses. Based on self-reported results, using the same test, over 81 percent had a positive response to the treatment. Of these, 12.8 percent reported that their symptoms were “basically gone,” over 41.3 percent reported that symptoms were decreased substantially, and 17.4 percent reported a slight decrease.
In 2016, another study was conducted to test the effectiveness of the neurolens approach specifically to treat digital eyestrain. Patients were screened for the study by means of a questionnaire about symptoms of digital eyestrain. Symptoms were ranked on a scale of 1 to 32; patients with scores of 6 or more who spent 10 hours per week or more on a computer were enrolled in the study (23 in all). Subjects received a subjective refraction from an optometrist and were tested using the neurolens Measurement Device. The results of the two tests were used to create eyewear with neurolenses.
Patients returned for follow-ups after 30 and 60 days. At each follow-up appointment, they were asked to fill out the CVS questionnaire once more. At the 30 day follow-up, they were tested using the neurolens Measurement Device with their glasses on, to see if further changes were needed after the patient had adjusted to the prism in the neurolenses. Seven patients received new lenses.
In a survey, 93 percent of patients responded positively to their neurolenses, and 82.5 percent indicated that they would recommend neurolenses to others (Fig. 8).
NEUROLENSES IN YOUR PRACTICE
The process of dispensing neurolenses involves every step in the patient’s journey through the practice. It begins in the reception area. When patients arrive, they should be asked to fill out a patient questionnaire or lifestyle index. This should ask specifically about the patient’s use of digital devices, and the symptoms of digital eyestrain, including headache, head and shoulder pain, and dry eye. According to The Vision Council study cited above, only about 10 percent of patients suffering from digital eyestrain report their symptoms to the doctor, probably because they don’t make the connection between the symptoms, their vision and digital device use. It is crucial then that the symptoms be uncovered so the eyecare professional can make the connection. A lifestyle index form is available from neurolens.
Next, if indicated, the patient can be tested using the neurolens Measurement Device. This can be done in the pre-test; as mentioned before; it only takes about three minutes. The results are provided to the doctor.
Direct involvement by the doctor is critical in recommending neurolenses. A recommendation from the doctor will always carry the most weight, but this is especially true of lenses that go beyond vision correction as such to address a neurological condition. It is most appropriate then to make the recommendation in the medical context of the exam room rather than the optical.
Patients need to know the following:
- The results of the neurolens Measurement Device test indicate that the patient has an alignment problem in the eyes that make binocular vision more challenging.
- This alignment problem is subtle and wouldn’t be visible by looking at the eyes.
- This alignment problem requires that the eye muscles make constant adjustments to maintain a binocular focus.
- These adjustments overstimulate a crucial nerve in the brain (the ophthalmic branch of the trigeminal nerve), which can cause headaches, neck and shoulder pain, and a sensation that they may perceive as dry eyes.
- The problem is most likely to be worse during extended viewing of a digital screen, which is a challenging visual environment.
- A new type of lens is available that will compensate for the misalignment of the eyes so that the eye muscles will require fewer adjustments.
- Most patients experience relief from their digital eyestrain symptoms.
In the exam room or during the fitting and dispensing process, it should be explained to the patient that neurolenses adjust the way the eyes communicate with the brain and that this requires an adaptation period. This adaptation period is similar to that experienced by the first time progressive lens wearer, although the adaptation period may be a bit longer.
 THE NEUROLENS
OPPORTUNITY
THE NEUROLENS
OPPORTUNITY
The benefits of offering a solution for digital eyestrain that for the first time diagnoses and addresses the root cause of the problem is invaluable to the many patients suffering from this condition. As such, any practice committed to delivering the highest standard of care will welcome a comprehensive diagnostic device and treatment for digital eyestrain with neurolens lenses.
The use of the neurolens Measurement Device is essential to determine the patient’s trigeminal dysphoria. Still, it also has the secondary benefit of building the patient’s confidence in the solution. A problem with any innovative lens technology is that patients don’t know that the lenses they have ordered will, in reality, be better until they receive their new glasses and try their new lenses. It requires a leap of faith for the patient. With neurolens, however, they get to experience the improvement that they can expect in their new lenses, before-hand. The test they will undergo is like none they have experienced before, giving them an (accurate) impression that the practice employs state-of-the-art technology, going above and beyond standard vision care. The test is an objective test of the vision issues underlying their symptoms. The patient experience with the neruolens Measurement Device lets them feel confident that they are doing the right thing in upgrading to neurolens.
Let’s conclude by returning to the result of the digital eyestrain study. The results were overwhelming: The vast majority of patients who received neurolenses reported that they were willing to recommend them to others. The experienced eyecare professional knows that word-of-mouth is the most potent form of marketing for any independent eyecare practice. Advocates for neurolenses will become advocates for your practice and promoters. The word will spread quickly as new patients seek relief from their digital eyestrain symptoms.

