By Palmer R. Cook, OD
“Heroes are made, not born,” is a saying popularized by cartoonist J. R. Williams in the middle of the last century. This may be debatable, but the star performers in my own practice and in many other practices are proven ophthalmic care heroes, and they often share certain traits. These traits commonly include: a strong interest in helping the patients with whom they work, a solid attention to detail and an enthusiastic approach to each day.
These star performers often are very effective in recognizing patient/practice problems before they become epic in scope. They also tend to be interested in developing an understanding of more than the superficial details of how their work relates to the needs of the patients they see. Most of all, they find their work challenging and personally rewarding beyond their bi-weekly paycheck—but of course, that’s important too.
We all would like to have as many star performers in our practices as possible. When someone joins your staff, they might not realize that they may be starting on a potentially interesting and a surely challenging road. You can help make that a road that leads to a satisfying career if you nurture that person’s interest with basic training that includes more than a description of duties and expectations.
HOW IT CAN HAPPEN
Your new hire was chosen on the basis of personality, ability to work well with others, a work history that included good attendance, ability to handle complex tasks, some computer skills and strong recommendations from previous employers. She had researched eyecare enough to demonstrate some knowledge of the three Os when interviewed. But she had neither experience nor training in eyecare. You feel that she has good potential to become a key member of your staff and a long-term asset to your practice. She is a prime candidate for basic training.
ORIENTATION
Whether a new hire is new to eyecare or not, an orientation including a rules-of-the-road discussion about office etiquette and performance expectations with the office manager or owner is a good first step. This can be followed by a combination of a “shadowing” of various staff members so the new hire can observe, several periods of one-on-one orientation with other staff members describing their skills and duties, and some regularly scheduled basic training sessions. Even if a new hire has previously worked in an eyecare practice, don’t assume that he or she has the depth of understanding that will serve your practice well. Every employee deserves some form of orientation when they come on board, but an orientation is a different sort of training that usually does not include much foundation information.
LENS BASICS
Lenses are used in eye exams. Patients purchase and enjoy the benefits their lenses provide. Prescriptions are written for lenses. It makes sense that anyone new to your practice might want to know some basic information about these useful and often misunderstood products.
The universe of vision care can be confusing, baffling and seemingly contradictory at any level. At the entry level, these problems can seem exponentially amplified. There is no simple starting point. However, if you begin with a couple of spherical lens blanks, one around a +6.00 and the other about a –6.00, a square plano prism of about 2Δ and a laser pointer, your student will be less apprehensive than if you began with an anatomical model of an eye, or a series of slides showing the visual pathways. After all, lenses are just curved pieces of clear material with no wires, buttons, gears or circuit boards.
You might begin by pointing out that all lenses for vision problems are either plus lenses, which add power to the eye, or minus lenses with subtract power from the eye. Or in some cases, they are plano (or zero optical power) lenses that neither add nor subtract optical power from the eye, but which are used for eye protection or filtering purposes.
Plus lenses are always thicker in the center and thinner on the edges, and minus lenses are always thinner in the center and thicker on the edges. When your student handles your lens samples, it will be easy for him or her to see this very basic fact of lens anatomy. It’s important to keep in mind that up to this point, your student, just like most people outside of our industry, sees all glasses as being essentially the same (except perhaps for cost and the style of the frame).
Cut two notches 180 degrees apart in the lip of a plastic foam coffee cup. Then put a laser pointer in the notches taped or wrapped by a rubber band so the light stays on. Draw a black circle about the size of a quarter in the center of a piece of copy paper, and tape the paper on a wall a few feet from your desk positioned so the laser light is centered in the circle.
Let your student know that the optical center of any lens is the point that gives the best optical performance the lens has to offer. Also, light passing through the optical center of a lens is not bent. This is easily demonstrated by holding the lens so that the laser spot stays within the black circle. If the lens is minus power, the laser spot will move to the left as you move the lens to the right, and to the right as you move the lens to the left (“against motion”), and when the plus lens is demonstrated “with motion” will occur. If you position the lens so the laser beam is in the black circle, that beam will be passing through the optical center of the lens. The light is always bent more and more toward the thickest part of the lens as the laser ray moves further away from the optical center. This an ideal way to introduce the concept of prism and the relationship of the lens’ power to the prism effect away from center (i.e., Prentice’s Law).
The above demonstration opens the door to explaining how patients with eye-aiming problems can be given lenses with prism to reposition whatever they are viewing so that it takes less effort to use both eyes together as a team. Use the plano, square prism to show how the laser spot jumps when the light passes through it. Then give your student some reading material, and put the prism (BO) in front of one of her eyes. She will probably notice little interference with her reading when you do this. Then as she continues reading, place the prism again in front of one of her eyes, but this time base up (BU) or base down (BD). Point out that the same prism worked quite differently depending on its position. Most people find this demonstration memorable. It is a demonstration that clearly shows the impact of an eye muscle problem or an incorrectly fabricated lens.
You might also show how objects seen through a plus lens move in a direction opposite to the movement of the lens, and for minus lenses the objects will move in the same direction as the lens. This gives another method for identifying whether a lens is either plus or minus.
PRISM
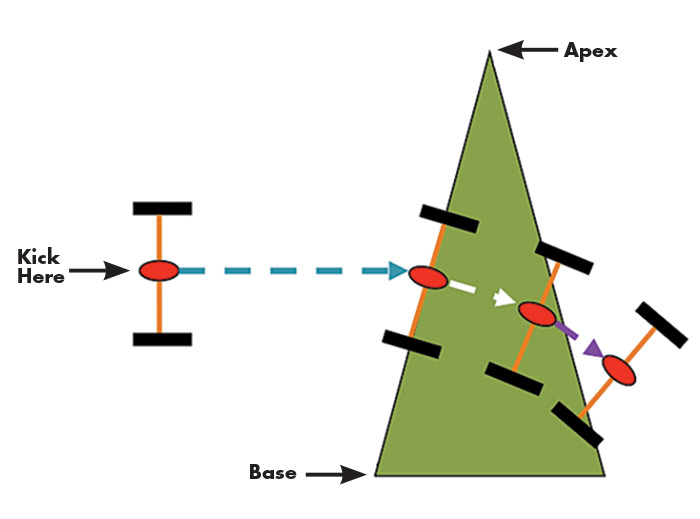
The speed of light is constant. It travels at about 186,000 miles a second. But that is only true in a vacuum. When light travels through other materials it slows down. For example, a standard plastic lens will slow light down to a little over 124,000 miles per second when the light ray enters the lens. That ray will poke along at that reduced speed until it exits the other side of the lens. As it exits, it performs one of nature’s most mysterious tricks of putting the pedal to the metal and speeding right back up to 186,000 miles per second. See Fig. 1 to visualize how this makes a kind of lens called a prism work.
The top of the “yard” which represents a prism in Fig. 1 is called the apex of the prism, and the wider part at the bottom of the prism is called the base of the prism. Light entering a prism is always bent toward the base of the prism. Prisms are most often prescribed when the eyes don’t aim properly. When eye aiming is a problem, one eye usually points toward what the person wants to see, and the other eye points in some other direction. In such cases, prism lenses, because they change the direction of the light flow, can be used so that even though the eye is turned, the image is moved to allow both eyes to view the same object.
LENS PRESCRIPTIONS
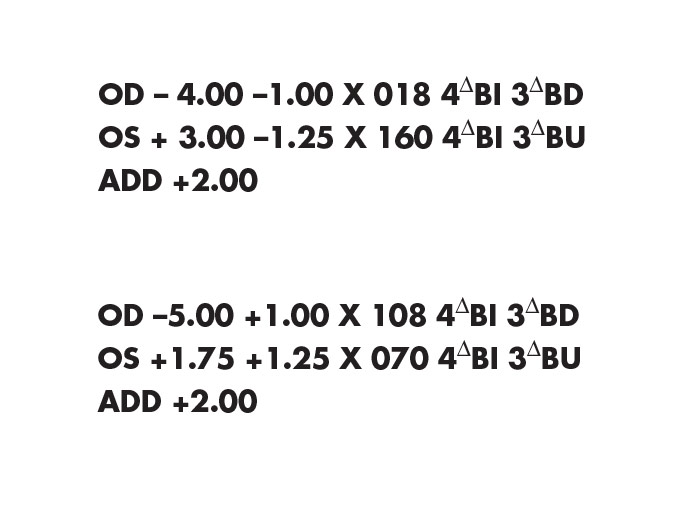
Lens prescriptions are usually just power formulas that tell how much optical power must be added or subtracted from each of the patient’s eyes (Fig. 2). The OD notation stands for “right eye” and comes from the Latin term oculus dexter. The right eye is listed first. OS stands for “left eye” from the Latin, oculus sinister. The first set of numbers moving from left to right are called the sphere power of the lens, with a minus sign indicating optical power was overall to be subtracted from the eye and with a plus sign indicating optical power was overall to be added to the eye. In some cases, an expiration date is included, beyond which the prescription should not be refilled. Some optometric state boards require that a PD must be given, although this is seldom the monocular PDs that should be used for eyewear fabrication. Monocular PDs are not needed for eye exams, and they can only be measured correctly after the frame has been fitted.
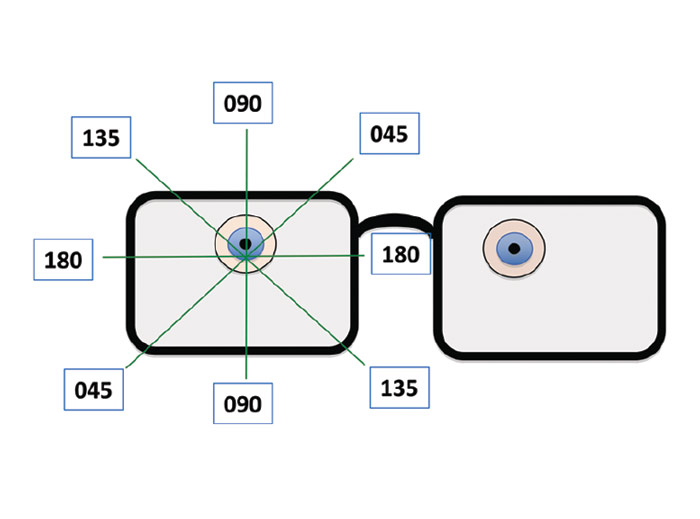
If there is a second set of numbers followed by an “x” in the lens formula, they will always be minus if the prescription is written in minus cylinder form. In plus cylinder form, any second set of numbers followed by an “x” will always be plus. A simple cylinder will have no power in its axis meridian, and it will have its maximum power 90 degrees from the axis meridian. If you think of a roll of paper towels lying on a table, the steepest curve of the roll will be vertical, and the flattest contour of the roll will be horizontal. If you want to spin the roll to release some towels, you can use a broomstick as an axle (or axis) around which the roll can spin. The symbol “x” stands for axis in lens formulas, and the next set of numbers to the left would be the meridian (Fig. 3) in which the doctor wants the axis of the cylinder to be positioned (a horizontal axis would be a line running from 0 to 180 on a protractor, but for lenses and eyes the horizontal axis is always marked 180. For axis positions from 001 through 099, three digits should always be used. Otherwise, the optician may be unsure if 18 or 180 was intended, or if “1” should have been 100 to 180, 010 to 019, or 001. People get interrupted in a busy office so be wary if three digits aren’t there.
The numbers that are followed by a Δ symbol, indicate that the patient needs prism which is usually prescribed to give patients comfortable binocular vision. BI means the prism should be oriented with its base inward toward his nose, and BO means the prism should be oriented with its base turned outward, away from his nose. BI and BO prisms are called lateral prisms, and when they are used they are most often BI in both eyes or BO in both eyes. BD means the base of the prism should be downward, and BU means the base of the prism should be upward. BD and BU prisms are called vertical prisms, and if BU is specified in one eye, most often, BD will be specified in the other.
The final part of many prescriptions is the Add. The Add notation tells the optician that the patient needs more plus power or less minus power for close work. An Add is sometimes prescribed for children to relieve eye muscle problems related to over-convergence while reading.
Interestingly, the custom of shaking hands, which dates back to the time of ancient Greece, tied up the right hand, leaving left-handed people an opportunity to draw a short sword or dagger. Could that be the reason sinister grew into a word indicating evil or threatening? For our purposes, the left eye is neither more nor less sinister than the right, other than for its name.
LENS MATERIALS
All staff members should have some understanding of lens materials. We no longer live in an eyecare world of either plastic or crown glass. There are many fine ophthalmic lens materials on the market. Patients who all want: A. To See Well, B. To Look Good, and C. To Be Comfortable, can be benefited by a careful selection of the best material for their needs.
Crown glass is the most scratch resistant material, but it is approximately twice as heavy as the most widely used plastic lens material (1.49 or standard plastic). Among the plastic lenses the Trivex, Trilogy and Phoenix family of materials from PPG are the lightest weight choice for prescriptions between about -11 to +12 diopters in power, but in the highest powers they are thicker than some other materials. Polycarbonate (poly) and the Trivex materials are similarly impact resistant. Poly has higher reflectance and lower optical performance, and Trivex materials are more costly to produce, but they perform better optically.
For higher powers of lenses, the materials with indices of 1.60, 1.66/1.67, 1.74 and even higher will have increased reflectance, but as you go up the index scale, each step higher also means some reduction in thickness. Sketching a diagram similar to Fig. 1 can help your student visualize how lens materials bend light. The small grassy area that impedes the wheels in this diagram would have grass like the greens on a golf course for a low index material, grass similar to a yard in need of attention for mid-index materials and perhaps foot-high weeds for a really high index material. The benefit of the higher index materials is that they have more “light bending muscle,” and therefore, the lenses can be made thinner and with less highly curved surfaces. Of course, the difference between a simple prism with flat lens surfaces and a lens with refractive power is that parallel rays entering the prism will emerge deviated, but still parallel, while parallel rays entering a lens with refractive power will emerge converging or diverging.
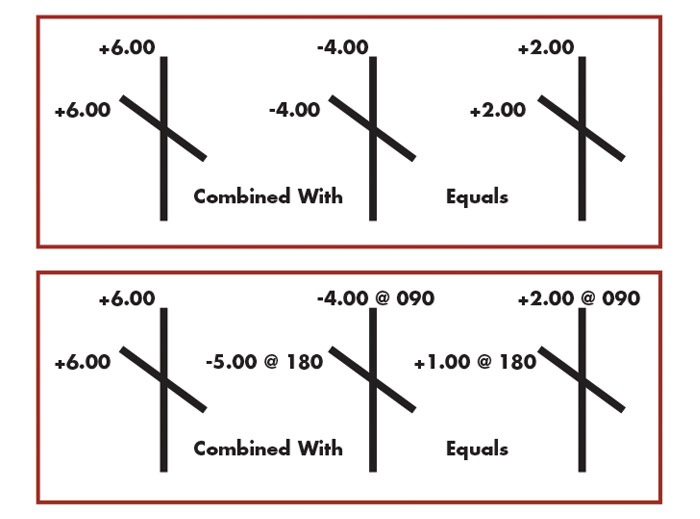
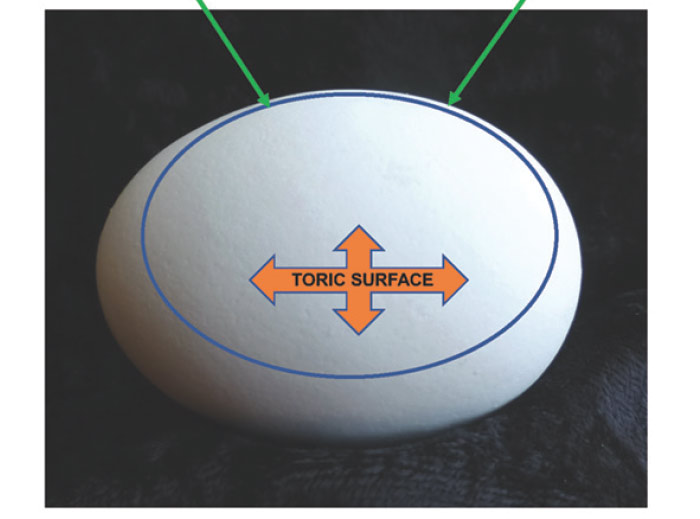
It can be helpful at this point to describe the map that identifies the 180 meridians of both the eye and all ophthalmic lenses (Fig. 3). This is a more or less painless way of introducing the concept of toric curves and the dreaded term, astigmatism. Although you are not laying the groundwork to make your new staff member an optician, explaining the Major Meridians of toric lenses can open the door for using optical crosses to represent lenses. This is a shorthand that most people find easy to understand (Fig. 4). Every lens that is used for correcting astigmatism has two major meridians. One is the meridian of the axis of the cylinder, and the other is located 90 degrees from the axis of the cylinder.
THE EGG AND EYE
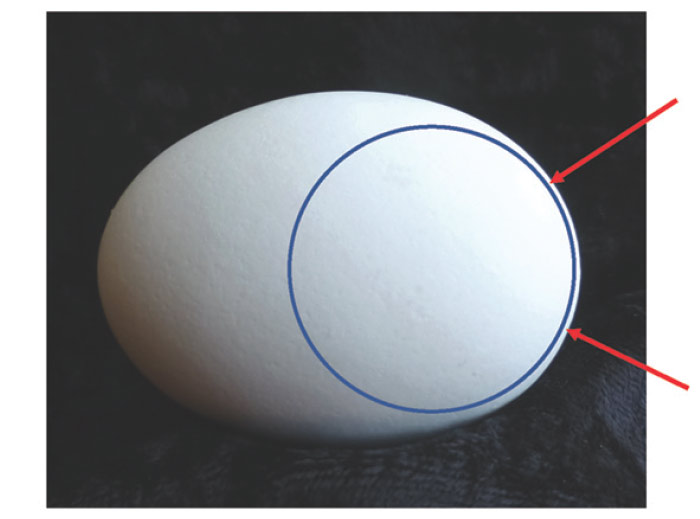
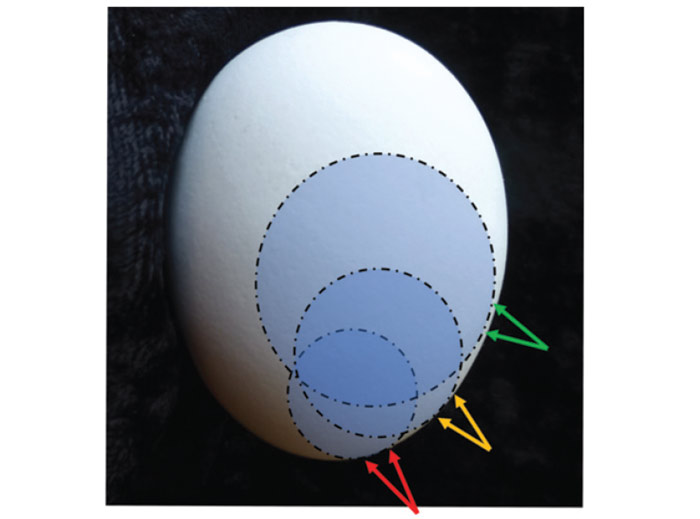
The rounded bottom of a chicken’s egg nicely shows a spherical curvature (Fig. 5a), and the other end of the egg is also spherical, but much more steeply curved. The surface of an egg about halfway from one end to the other is clearly a toric surface similar to the shape of the cornea’s when with-the-rule astigmatism is present (Fig. 5b). The principle underlying how plus power is added to PALs for reading is shown in (Fig. 5c). Although a chicken’s egg has steeper curvatures than most ophthalmic lenses, a lens clock can be used for demonstration purposes (Fig. 5d).
OCULAR ANATOMY AND FUNCTION 101
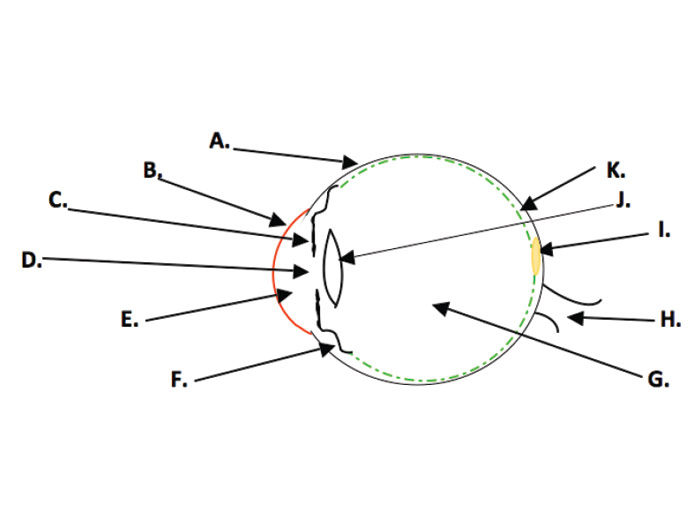
The optical portion of the eye includes the cornea, pupil, lens and the transparent aqueous and vitreous. The retina, which lines the inside of the eye, functions as a transducer(Fig. 6). Transducers convert one form of energy into another. In the retina, optical energy is transformed into electrical energy which is then transmitted via the optic nerve and other structures to the areas of the brain that provide us with a construct of the world around us.
In order to send electrical impulses that allow the best percept of the external world, a clear image must be formed on the retina. For a “normal” eye, that means that the light rays from about 20 feet or more away must be bent by a total optical power of about 62 diopters. The cornea supplies about 42.5 diopters of the needed power, and the lens of the eye supplies about 19.5 diopters of the remainder.
REFRACTIVE ERROR
The primary motivator causing people to seek eyecare in the U.S. is probably refractive error. Refractive error includes myopia (nearsightedness), hyperopia (farsightedness), astigmatism and in the strictest sense presbyopia. Refractive error means that the optical parts of the eye do not form a clear image on the retina when the focusing mechanism (accommodation) is relaxed. This can be due to the optical power of the eye being too strong, or too weak in some or all of the meridians of the eye. If the optical power of the eye is inappropriate, the refractive error is termed a refractive refractive error. If the eye is physically too long or too short from front to back, the condition is called an axial refractive error. Spectacle lenses, contact lenses and surgery have all been used to correct refractive error.
PHORIAS AND TROPIAS
There are six eye aiming muscles wrapped around each eye. They are called the extraocular muscles. Four of these muscles primarily turn the eye upward, downward, to the right or to the left. The other two muscles primarily rotate the eye clockwise or counterclockwise. If for any reason these muscles do not work well as a team, your patient will have to use extra effort to aim both eyes properly. This condition is called a phoria. If you cover one eye as you look at a clock across the room, that eye may stay perfectly aligned with the other eye, but for most people it will drift to a position of rest, perhaps a bit to the right, left, above or below the clock you are viewing. If you then move your hand to cover the other eye while still looking at the clock, you may see the clock apparently jump a bit toward the right or left, or even upward or downward. A small amount of movement indicates a tendency, which you are controlling by the use of your extraocular muscles, for one eye to turn from your intended direction of gaze. Small amounts of phoria do not cause problems and don’t require treatment. Moderate amounts of phoria can cause ocular discomfort, reading problems and avoidance of prolonged tasks requiring close visual attention. Certain kinds of eye exercises or prism lenses, or both may be needed if the phoria causes problems.
A tropia is a condition in which the eye muscles or the nerves supplying them cause one eye to be primarily used for vision and the other deviates so that it is not pointed at the same object of regard as the preferred eye. Tropias are sometimes correctable with special eye exercises, the use of prism or eye muscle surgery. Often a combination of these approaches is needed to correct the tropia. Another word for tropia is strabismus. Tropias can be constant, intermittent or alternating (i.e., sometimes the right eye is preferred, and other times the left eye is preferred). Tropias can be small angle (i.e., the eyes are nearly in alignment) and hard to detect, or wide angle in which the condition is obvious and often cosmetically unacceptable. In medieval times a drifting eye was sometimes referred to as an “evil eye.”
APOLOGIES, THOUGHTS AND SUGGESTIONS
First, my apologies to experienced and vision care savvy readers: As you are already aware, there is considerable “rounding” and simplification of the information presented here. The above comments are to help you orient someone entering an eyecare practice. Make your basic training manageable for your student. Although this is familiar ground to you, a lengthy session could leave your new employee feeling as though he or she had been trying to drink from a fire hydrant.
Approach the material as a discussion, and give plenty of opportunity for your new employee to ask questions. Inject your own experience into the discussion, and be sure your student knows there is no expectation of all the material being completely absorbed. Ask a few questions as you go through each part of the material, and pace your presentation accordingly. Once-over-lightly as you do a series of 30 to 45-minute sessions is a good rule. After 90 days on the job, when roots have begun to sink in, you can repeat and elaborate as a refresher. Hopefully, you will see the emergence of a new eyecare hero starting within your practice.
GLOSSARY OF BASIC OPTICAL TERMS
ACCOMMODATION: The lens of the eye is designed to change shape so that the eye’s optical power is increased for seeing close objects. This process is called accommodation. Accommodation results from contraction of the ciliary body which allows the lens to change to a more curved shape (i.e., provide more optical power to the eye).
Astigmatism: This is a condition in which the contours that make up the images that should fall flat on the retina are focused at varying distances from the retina. Moderate to larger amounts of astigmatism cause blur, but astigmatism in smaller amounts may cause strain with relatively little blur.
DIOPTER: A diopter is a unit of light bending power. One diopter is the amount of light bending power that can bend parallel rays of light to a focus 1 meter (about 39 inches) from the lens. All lenses, eyes and optical instruments have light bending power measured in diopters.
HYPEROPIA: Commonly called “farsightedness,” this is a condition in which the image of distant objects formed by the eye, when accommodation is relaxed, is blocked by the back of the eye before it can come to a focus. Hyperopia causes strain at all distances, especially for near work. Hyperopia can be associated with reading difficulties, ocular discomfort and frequent styes or lid infections.
INDEX: The light bending power of every lens material is assigned a number (e.g., 1.49, 1.53, 1.60, 1.66, 1.67, 1.70, 1.74, etc.) that gives its ability to bend light of a given wavelength. A lower index number means a lens of a given power and shape must be more steeply curved and have greater volume than if it were made of a higher index material.
Myopia: Commonly called “nearsightedness,” this is a condition in which the image of distant objects formed by the eye, when accommodation is relaxed, falls in front of the retina. Myopia causes blur at far distances, but near vision may be clear.
PD: The PD is the shortest distance between the points at which the right and left lines-of-sight intersect the lenses of a properly adjusted frame when the patient’s level lines-of-sight are parallel and an object on the patient’s mid-line is being viewed.
NEAR PD: The near PD is the distance between the points at which the right and left lines-of-sight intersect the lenses of a properly adjusted frame when the patient’s lines-of-sight are directed at an object on the patient’s mid-line and which is located at a comfortable distance for near work (usually 40 cm).
HALF PD: The half PD is the distance from the center of the bridge of the properly adjusted frame to the point at which the line-of-sight intersects the lens when a distant object on the patient’s mid-line is being viewed.
MONOCULAR PD: The monocular PD is the shortest horizontal distance from the point at which the line-of-sight intersects the lens to a vertical line extending downward from the center of the properly adjusted frame when an object at near (usually 40 cm from the spectacle plane) and located on the patient’s mid-line is being viewed.
OPTICAL CENTER: The optical center of a lens is that point in a lens through which an entering ray at right angles to the lens surface will pass undeviated.
PRISM: A simple prism causes light rays to change direction (Fig. 1), but does not bring light to a focus. Objects viewed through a prism appear to be displaced from their real location.
PRISM DIOPTER: A prism diopter is a unit of measurement used to indicate the amount of deviation that occurs when light passes through a prism. A one prism diopter prism (1Δ) deviates a light ray 1 cm at a distance of 1 meter from the lens.
Prentice’s Law: This law states that a light ray passing through a lens will be deviated by an amount in prism diopters equal to the distance in centimeters from the optical center of the lens to the point of intersection at which the ray enters the lens times the power of the lens in diopters. For example, if a light ray enters a 4.00 diopter lens 1 cm from the optical center, it will be deviated by 4 prism diopters (1cm x 4.00 diopters).
PRESBYOPIA: The lens, which grows layer upon layer as birthdays pass, eventually loses its ability to reshape (accommodation) enough to allow clear vision at normal reading distances. This usually is first noticed in the fourth decade of life, and the early symptoms often include a need to hold reading material further out, a requirement for added light for near tasks and considerable annoyance accompanied by a desire for the vision of youth. Reading glasses, bifocals, bifocal contacts, progressive addition lenses (PALs) and sometimes correcting one eye for distance and the other for near with contact lenses, called “monovision” are among the systems that are used for compensating for presbyopia.
ACCOMMODATION: The lens of the eye is designed to change shape so that the eye’s optical power is increased for seeing close objects. This process is called accommodation. Accommodation results from contraction of the ciliary body which allows the lens to change to a more curved shape (i.e., provide more optical power to the eye).
Astigmatism: This is a condition in which the contours that make up the images that should fall flat on the retina are focused at varying distances from the retina. Moderate to larger amounts of astigmatism cause blur, but astigmatism in smaller amounts may cause strain with relatively little blur.
DIOPTER: A diopter is a unit of light bending power. One diopter is the amount of light bending power that can bend parallel rays of light to a focus 1 meter (about 39 inches) from the lens. All lenses, eyes and optical instruments have light bending power measured in diopters.
HYPEROPIA: Commonly called “farsightedness,” this is a condition in which the image of distant objects formed by the eye, when accommodation is relaxed, is blocked by the back of the eye before it can come to a focus. Hyperopia causes strain at all distances, especially for near work. Hyperopia can be associated with reading difficulties, ocular discomfort and frequent styes or lid infections.
INDEX: The light bending power of every lens material is assigned a number (e.g., 1.49, 1.53, 1.60, 1.66, 1.67, 1.70, 1.74, etc.) that gives its ability to bend light of a given wavelength. A lower index number means a lens of a given power and shape must be more steeply curved and have greater volume than if it were made of a higher index material.
Myopia: Commonly called “nearsightedness,” this is a condition in which the image of distant objects formed by the eye, when accommodation is relaxed, falls in front of the retina. Myopia causes blur at far distances, but near vision may be clear.
PD: The PD is the shortest distance between the points at which the right and left lines-of-sight intersect the lenses of a properly adjusted frame when the patient’s level lines-of-sight are parallel and an object on the patient’s mid-line is being viewed.
NEAR PD: The near PD is the distance between the points at which the right and left lines-of-sight intersect the lenses of a properly adjusted frame when the patient’s lines-of-sight are directed at an object on the patient’s mid-line and which is located at a comfortable distance for near work (usually 40 cm).
HALF PD: The half PD is the distance from the center of the bridge of the properly adjusted frame to the point at which the line-of-sight intersects the lens when a distant object on the patient’s mid-line is being viewed.
MONOCULAR PD: The monocular PD is the shortest horizontal distance from the point at which the line-of-sight intersects the lens to a vertical line extending downward from the center of the properly adjusted frame when an object at near (usually 40 cm from the spectacle plane) and located on the patient’s mid-line is being viewed.
OPTICAL CENTER: The optical center of a lens is that point in a lens through which an entering ray at right angles to the lens surface will pass undeviated.
PRISM: A simple prism causes light rays to change direction (Fig. 1), but does not bring light to a focus. Objects viewed through a prism appear to be displaced from their real location.
PRISM DIOPTER: A prism diopter is a unit of measurement used to indicate the amount of deviation that occurs when light passes through a prism. A one prism diopter prism (1Δ) deviates a light ray 1 cm at a distance of 1 meter from the lens.
Prentice’s Law: This law states that a light ray passing through a lens will be deviated by an amount in prism diopters equal to the distance in centimeters from the optical center of the lens to the point of intersection at which the ray enters the lens times the power of the lens in diopters. For example, if a light ray enters a 4.00 diopter lens 1 cm from the optical center, it will be deviated by 4 prism diopters (1cm x 4.00 diopters).
PRESBYOPIA: The lens, which grows layer upon layer as birthdays pass, eventually loses its ability to reshape (accommodation) enough to allow clear vision at normal reading distances. This usually is first noticed in the fourth decade of life, and the early symptoms often include a need to hold reading material further out, a requirement for added light for near tasks and considerable annoyance accompanied by a desire for the vision of youth. Reading glasses, bifocals, bifocal contacts, progressive addition lenses (PALs) and sometimes correcting one eye for distance and the other for near with contact lenses, called “monovision” are among the systems that are used for compensating for presbyopia.
Contributing editor Palmer R. Cook, OD, is an optometric educator and optical dispensing expert.