Healthy Tear Film with Warm Eyes
By Deborah Kotob, ABOM
Learning Objectives:
Upon completion of this program, the participant should be able to:
- Explain the three layers of the tear film and describe their function.
- Describe Meibomian Gland Dysfunction as the number one cause of chronic dry eye.
- Explain how warm compression of the lids expresses the clogged oils from the meibomian glands.
Faculty/Editorial Board
 Deborah Kotob, ABOM, is the Director of Education and Training for Jobson Medical Information. Her experience spans more than twenty years in the optical industry. During this time, her roles included optical boutiques owner, optician, optical frame sales, and over ten years in lens manufacturing as a Lens Consultant, Trainer, and LMS content developer. She lectures, trains, conducts webinars on a variety of optical and practice development topics.
Deborah Kotob, ABOM, is the Director of Education and Training for Jobson Medical Information. Her experience spans more than twenty years in the optical industry. During this time, her roles included optical boutiques owner, optician, optical frame sales, and over ten years in lens manufacturing as a Lens Consultant, Trainer, and LMS content developer. She lectures, trains, conducts webinars on a variety of optical and practice development topics.
Credit Statement
This course is approved for one (1) hour of CE credit the American Board of Opticianry (ABO). One hour, Ophthalmic Level 2, Course number: STWJHI071-2
Support
This is a product spotlight CE supported by an educational grant from ZEISS.

If you are one of the estimated 45 million Americans suffering from dry eye disease, the frustration with ineffective, inconvenient treatments is enough to bring you to tears! But do not confuse reflex tears when you cry with basal tears of the eyes tear film. Reflex tears are produced in response to pain or emotion, while basal tears protect the ocular surface and keep the cornea healthy and moisturized for visual clarity.
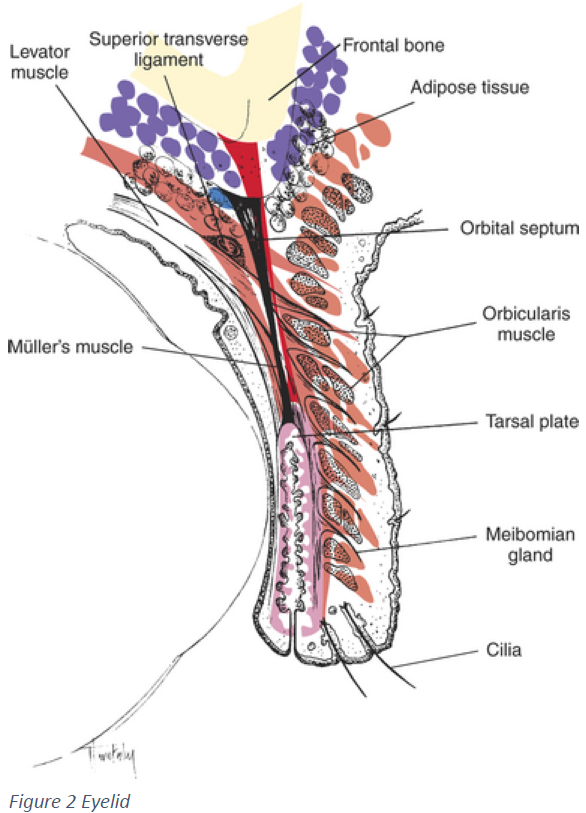
Today, we are addressing the effect of our meibomian glands in our eyelids on the quality of basal tears and the link to chronic dry eye disease (DED). (Fig. 2) Also, we are introducing a new tool for the dry eye sufferer that allows them to increase the normal flow of meibum, the lipid layer of the tear film, to prevent evaporative dry eye disease. The Warm Eye Mask by ZEISS helps patients comply with at-home treatment protocols prescribed by their doctor by being easy, convenient, and effective. Compliance is one of the most cited frustrations for doctors and patients. I would know as I suffer from meibomian gland dysfunction, and the only treatment I was offered in the early stages was eye drops and a recommendation to apply warm compresses to my lids daily. I was frustrated and did not comply with daily warm compresses because there was no easy, convenient, and effective way to warm the eyes then. Until now, little has improved in the effectiveness or convenience of at-home warm compression tools.
Tear Film & Ocular Surface Society (TFOS) launched the TFOS Dry Eye Workshop II (TFOS DEWS II) in March 2015. The following is a quote from the TFOS DEWS II executive summary: "On the basis of peer-reviewed literature, the Tear Film Ocular Surface Dry Eye Workshop TFOS DEWS II Pathophysiology Subcommittee concluded that the core mechanism of DED is evaporation-induced tear hyperosmolarity, which is the hallmark of the disease. It damages the ocular surface both directly and by initiating inflammation. The cycle of events is described as the vicious Circle of DED. … At least 350 million persons worldwide, and in some Asian countries as many as 70% of their population, have dry eye. Meibomian Gland Dysfunction (MGD) is a major factor in nearly 90% of cases." according to TFOS DEWS II Report Executive Summary www.theocularsurface.com"
Dry eye affects young and old. While we see an upsurge in young digital natives experiencing dry eye, the risk, complications, and severity increase with age. A contributing factor in digital eye discomfort is dry eye resulting from not blinking when staring at screens. We need to blink to distribute our tear film over our eyes. But for our blinks to do their job, the tear film must be healthy. Dry eye is a progressive disease, not merely an annoyance, as many young people in the early stages believe. Unaware of dry eye's seriousness and progressive nature, they self-medicate with OTC eye drops. But OTC drops can mask the symptoms, allowing the disease to advance, treating symptoms but not the cause or halting the progression to the disease. Finally, out of desperation, we visit our ECP to find a permanent solution to end our eye irritation and pain. The discomfort we experience from dry eyes degrades our quality of Figure 2 Eyelid life and can ultimately affect our vision. As the disease progresses, more and more complications arise, ranging from chronic blepharitis, meibomian gland dysfunction, lid, and tear film abnormalities. Tear film abnormalities can cause too many of the wrong tears or insufficient quality tears. A healthy tear film nourishes, protects, and lubricates the eye to maintain the homeostasis of the ocular surface.
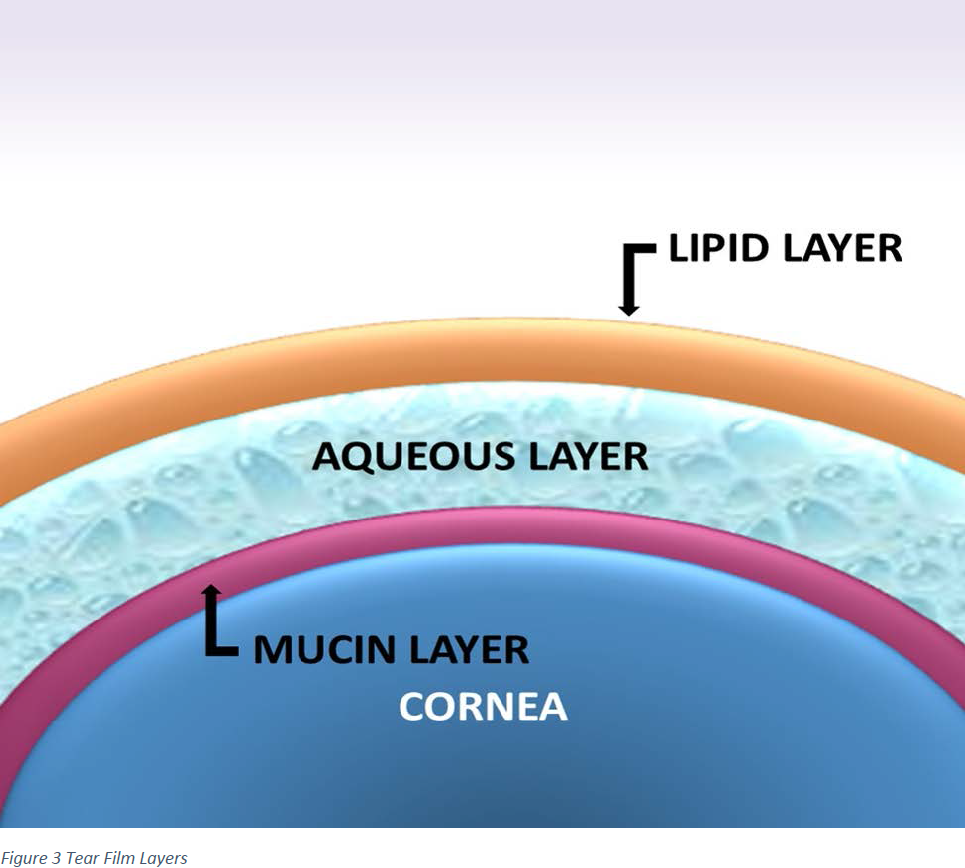
Our tear film comprises three layers whose acronym is LAM for Lipid layer, Aqueous layer, and Mucin layer. (Fig. 3) The stable equilibrium of these layers is vital for a healthy tear film. Without the correct amount of lipids, our tear film will evaporate. Without the correct number of mucins, our tears will not adhere to our eyes and spill over. Our tears will not be plentiful enough without the right amount of aqueous fluid. Every time we blink, the lids spread a healthy tear film over the cornea, washing away debris and nourishing the anterior eye. When the balance of the tear film is compromised, it can lead to dry eye disease (DED). There are many causes and contributing factors to dry eye disease, but the most common cause is meibomian gland dysfunction (MGD).
The importance of Meibomian Glands (MGs) in maintaining a healthy tear film and their link to ocular surface disorder or dry eye have recently gained attention. Dry eye treatment protocols have shifted rapidly to focus on the oil (meibum) layer in addition to watery (aqueous) tears. Efforts have been made, and products have been introduced to apply heat and pressure to the glands to melt oil blockages and allow meibum to flow freely once again.
When it comes to a healthy tear film, both the quantity and quality of the tears matter. Our normal tear film bathes our ocular surface, including the cornea, in moisture and nutrients with every blink. Dry eye occurs when our lacrimal glands do not make enough tears or the tear film evaporates too quickly because the quality of the tear film is poor. Without the proper balance of water, oil, and proteins (mucins), our tear film cannot moisturize, clean, and protect the ocular surface. So, when we have dry eye disease, we either do not make enough tears or produce good tear film quality. This tear film instability can lead to inflammation and damage to the ocular surface. Dry eye disease is a type of ocular surface disease.
The many contributing factors to dry eye include medication side effects (i.e., oral antihistamine or blood pressure meds), a dry, dusty, or smokey environment, or not blinking for long periods such as long hours staring at digital screens. Dry eye from contact lens use has its name, CLIDE, for contact lens-induced dry eye. All are modifiable factors that contribute to dry eye. Still, other common causes such as aging, eye surgery, and effects from underlying conditions (thyroid, diabetes, rheumatoid arthritis, Sjogren's syndrome, or Parkinson's) can be more difficult to correct. The following are the most common causes of ocular surface dysfunction: meibomian gland dysfunction (MGD), Anterior blepharitis, allergic conjunctivitis, and anterior uveitis.
Fortunately, the optical industry has stepped up, and more practices now specialize in dry eye treatment. Treatment is a multi-prong approach depending on the cause, which aims to reduce inflammation and restore the integrity of the tear film. If you are experiencing dry eye symptoms, get a comprehensive eye evaluation by an optometrist or ophthalmologist specializing in dry eye. Dry eye does not get better on its own and can become a chronic condition requiring long-term treatment. Dry eye is more successfully treated in the early stages and is a multi-faceted approach. Self-treating with over-the-counter lubricating drops may mask serious conditions by reducing symptoms; however, it does not treat the problem.
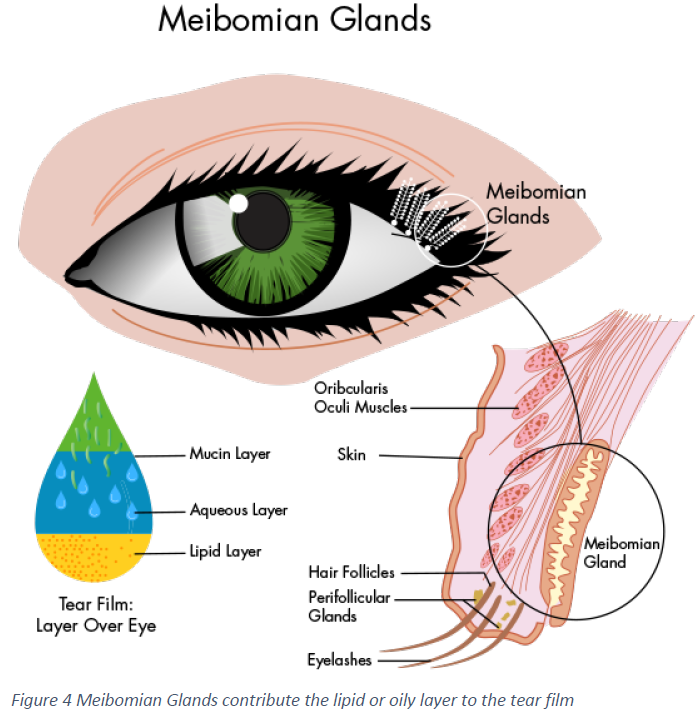
The meibomian glands are oil-producing in both your upper and lower eyelids. (Fig. 4) The oil these glands produce forms the outermost layer of your tear film. This oil layer protects your tears from rapidly evaporating. When these oils are reduced or eliminated, your tears evaporate from the surface of your eyes quickly, and your eyes become much drier. This is especially true when you are engaged in visually intense tasks such as reading (books, magazines, newspapers), staring at a computer, cell phone, or tablet screen, watching television, driving, etc.
Meibomian glands contribute to the lipid or oily layer of the tear film, preventing it from evaporating and leaving the surface too dry. According to the American Optometric Association, if MGD is not treated, a more severe form of this ocular surface disease can develop. It can display symptoms that can alter the quality of life. Because MGD causes evaporative dry eye, the cornea can become desiccated and dry to a point where scar tissue can form. If MGD is chronic, it can cause the meibomian glands to atrophy. Once they are atrophied, making them function normally again is very difficult. MGD can develop into ocular rosacea, requiring more aggressive medical treatment.
Patients may not notice anything in the early stages, but if left untreated, MGD can cause eye symptoms. Clogged glands eventually disappear or drop out and become unable to make oils for a healthy tear film. Signs and symptoms of MGD include dryness, burning, itching, redness, stickiness or crusting, watering, blurry vision that comes and goes, and a foreign body sensation or the feeling that something (like dirt or sand) is in the eyes. Eyelid inflammation from MGD may also cause styes or chalazion, aka meibomian gland cysts, to form on the eyelids. These different signs and symptoms of MGD may come about slowly and be hard to detect visually.
One cannot speak about dry eye without addressing blink mechanics. Every blink spreads the thin tear film evenly over the ocular surface, lubricating, cleaning, nourishing, and preventing inflammation and infection. Without this, the cornea can be exposed to drying conditions too long after the tear breakup time and develop dry spots and inflammation. A vicious cycle occurs where more drying is followed by more symptoms and inflammation and then more drying. Many factors can contribute to dry eye disease; among the many factors, tear film destabilization due to low blink rate or poor blink mechanics plays a role. The number one cause of dry eye disease is meibomian gland dysfunction. These glands produce the lipid layer of the tear film, preventing basal tears from evaporating too quickly. Blinking produces more meibomian gland lipid secretions, increasing the lipid layer thickness. Blinking also allows tarsal goblet cell mucin distribution, the tear film layer responsible for tear film stability.
Those who spend prolonged periods using digital devices are prone to poor blinking habits and ocular surface drying from reduced blinking frequency. Regular blinking exercises throughout the day help form normal and complete blinking habit patterns. Regularly practicing blinking exercises allows us to be proactive in ensuring consistent tear replenishment. In addition, blink exercises improve ocular surface health by expressing the meibum from the meibomian glands so that our tear film has a healthy balance of lipids. We have all heard of the 20-20-20 rule recommendation to look in the distance (20 feet) every 20 minutes for 20 seconds. It may be helpful to add blinking exercises to this routine.
In DED, early intervention is a window of opportunity. Most teens and young adults are unaware that the visual discomfort they experience from staring at digital device screens may be dry eye symptoms. They are unaware of the window of opportunity to receive preventative interventions through their eye doctor, which may reduce the risk of progression to dry eye disease. While we cannot blame dry eye entirely on our incessant use of digital screens, doctors report more young patients of younger ages (even teens) presenting with dry eye symptoms of meibomian gland dysfunction, which they attribute at least in part to Increased screen time (average 8 hours daily) and contact lens wear.
In the Ageing and the natural history of dry eye disease: A prospective registry-based cross-sectional study, findings show: "… that each decade of life is, on average, associated with 24% increased odds of developing dry eye disease." In the study, signs of meibomian gland dysfunction emerged earlier in the natural history of disease progression, with the optimal prognostic cut-off ages for gland dropout, diminished meibum expressibility, and reduced lipid layer quality occurring in the third decade of life, between 24 and 29 years of age; the optimal predictive ages for lid wiper epitheliopathy, tear film instability, hyperosmolarity, and dry eye symptoms occurred during the fourth decade of life (31-38 years); while the optimal prognostic thresholds for signs of aqueous tear deficiency and ocular surface staining occurred in the fifth and sixth decades of life (46-52 years). Signs of meibomian gland dysfunction appeared earlier in the natural history of disease progression, and the brief delay prior to the development of other clinical dry eye signs might represent a window of opportunity for preventative interventions in the young adult age group."

Early detection and treatment and protective/preventative measures can prevent decades of exposure to environmental and physiological insults that cause oxidative stress of the ocular surface and tear film, disrupting normal basal tear production and tear film stability. Dry eye disease (DED) is a multifactorial degenerative, progressive disease of the tears and ocular surface. Tear film instability leads to visual discomfort and loss of visual clarity. With age, we experience a decline in our protective tear proteins and enzymes that prevent damage from pollutants, ultraviolet radiation, and other recognized threats such as ozone and chronic use of preserved eyedrops to treat glaucoma, according to researchers Sophia Seen and Louis Tong in their research paper titled Dry eye disease and oxidative stress. The authors of the study state: "… an imbalance between the level of reactive oxygen species (ROS) and the action of protective enzymes will lead to oxidative damage, and possibly inflammation." Oxidative stress is exacerbated by our body's natural decline with age in antioxidants needed to combat oxidative stress.
We can do our part by ensuring every young adult patient and parent of teenagers is aware that dry eye can be more than discomfort; it can progress to dry eye disease. Make them aware that there is a window of opportunity for teens and young adults through early intervention to reduce the risk of them or their child developing dry eye disease.
The ZEISS Warm Eye Mask can be used preemptively as well as therapeutically. Just as we brush and floss daily for oral health, applying moist, warm compresses daily to our lids keeps meibomian glands healthy and functional, and the bonus is it is soothing and relaxing.
Open, Apply, Relax - ZEISS Warm Eye Masks are individually wrapped for hygiene you can count on. Convenient pocket-sized sachets are ideal for use anywhere – at home or on the go. Open the sachet, place the mask over your eyes, sit back, and breathe easy. Enjoy for 15 to 20 minutes to get the full benefits. The ZEISS Warm Eyes Mask consists of a central core that gradually heats to the correct temperature when exposed to the air. It distributes heat gently for safe, effective results. Beneath the core is a breathable film that turns the heat from the central core into gentle, warming steam to protect the delicate eyelid. It regulates the temperature and allows moist heat to be released. The soft, flexible top and bottom of the ZEISS Warm Eye Mask add an extra layer of comfort and ensure a snug fit.

In her article in Review of Optometric Business titled, The At-Home Dry Eye Treatment a Dry Eye Powerhouse Practice Trusts, Mei Fleming, O.D., owner of Luminance Vision Optometry in Lafayette, CA, speaks to the importance of at-home treatments and shares patient's responses to the Warm Eyes Mask at-home treatment.
"I prescribe the ZEISS Warm Eye Mask as a way to alleviate uncomfortable symptoms of dry eyes, eyestrain and to treat an eyelid stye. These masks deliver gentle, moist heat, which research has shown to be more effective in unclogging eyelid meibomian glands than dry heat alone. Meibomian glands are responsible for producing the oil layer of healthy, moisturizing tears. This oil layer prevents tear evaporation and increases tear contact time to adequately moisten and nourish your eyes. In the case of a stye, which is an enlarged and severely clogged meibomian gland, the ZEISS Warm Eye Mask can be used effectively to unclog the gland.
ZEISS Warm Eye Masks are also convenient, portable, and easy to use. If you are busy or always on-the-go, these masks provide an instant treatment anywhere, any time. Anyone who uses digital devices or experiences uncomfortable eye symptoms can benefit from this new at-home treatment. Most at-home dry eye masks require a microwave or need to be plugged into a power outlet. ZEISS Warm Eye Masks are individually packaged and are ready to use immediately upon opening.
I currently prescribe and sell this product in my office to any patient experiencing eye strain or dry eye symptoms. I educate my patients about meibomian gland dysfunction and how this contributes to dry eyes. With clogged meibomian glands, tears evaporate very quickly leaving the eyes dry. Heating these glands regularly prevents clogging and allows these glands to perform the important function of producing the oil, which is the outermost layer of healthy, moisturizing tears.
At-home treatments such as the ZEISS Warm Eye Masks allow my patient to maximize the therapeutic effects of in-office dry eye treatments and extend relief of their dry eye symptoms. My patients are telling me the masks are helping them stay compliant with their at-home dry eye therapy for maintenance. And my patients enjoy the convenience of these masks. Effective at-home treatments like the ZEISS Warm Eye Mask make life better for my patients while creating a level of satisfaction that brings them back to our office again and again for care." Mei Flemming, O.D. (Fig. 6)
I have firsthand experience with poor-quality tear film due to meibomian gland dysfunction (MGD), and I, like others with dry eye disease, have tried every configuration of heating techniques to melt the lipids to unclog meibomian glands so that the oil component of the tear film will flow normally producing a healthy tear film. For those of us who suffer from dry eye disease, one of our chief complaints and roadblocks to treatment compliance is an effective means to apply moist heat for enough time to melt the congested lipids clogging our meibomian glands. Meibomian gland dysfunction is the number one cause of ocular surface disorder, aka dry eye disease. Clogged meibomian glands result in an imbalance in our tear film, leading to evaporative dry eye and ocular surface disease. Trust me when I tell you I have tried it all: wet washcloths that will not stay hot enough and wrinkle our under-eye skin. I have tried the stick in the microwave bead bags. I have tried tea bags and boiled eggs. Do not laugh; when you suffer from dry eye disease, you try everything and anything, but in the end, none of these methods are effective, convenient, and easy. Thanks to Warm Eyes Mask by ZEISS, I can comply with my at-home treatment plan. I, for one, am thrilled that there is finally a product that is effective, easy to use, and individually packaged so that I can take some with me when traveling.
ABO Disclaimer: The ABO does not endorse this or any product mentioned in continuing education courses.



